Getting dental implants can be a life-changing experience, restoring smiles and confidence. However, sometimes issues can arise, and one concern many patients encounter is gum recession around their dental implants. This can be unsettling, making you wonder why it’s happening and what can be done. If you’re experiencing or worried about the aesthetic and health implications of receding gums around your implants, you’re not alone. Understanding the dental implant gum recession causes is the first crucial step toward effective management and prevention. This comprehensive article delves into the various factors that contribute to this condition, offering insights into why it occurs and how it can be addressed, ensuring your valuable investment in dental health continues to thrive.
Key Takeaways
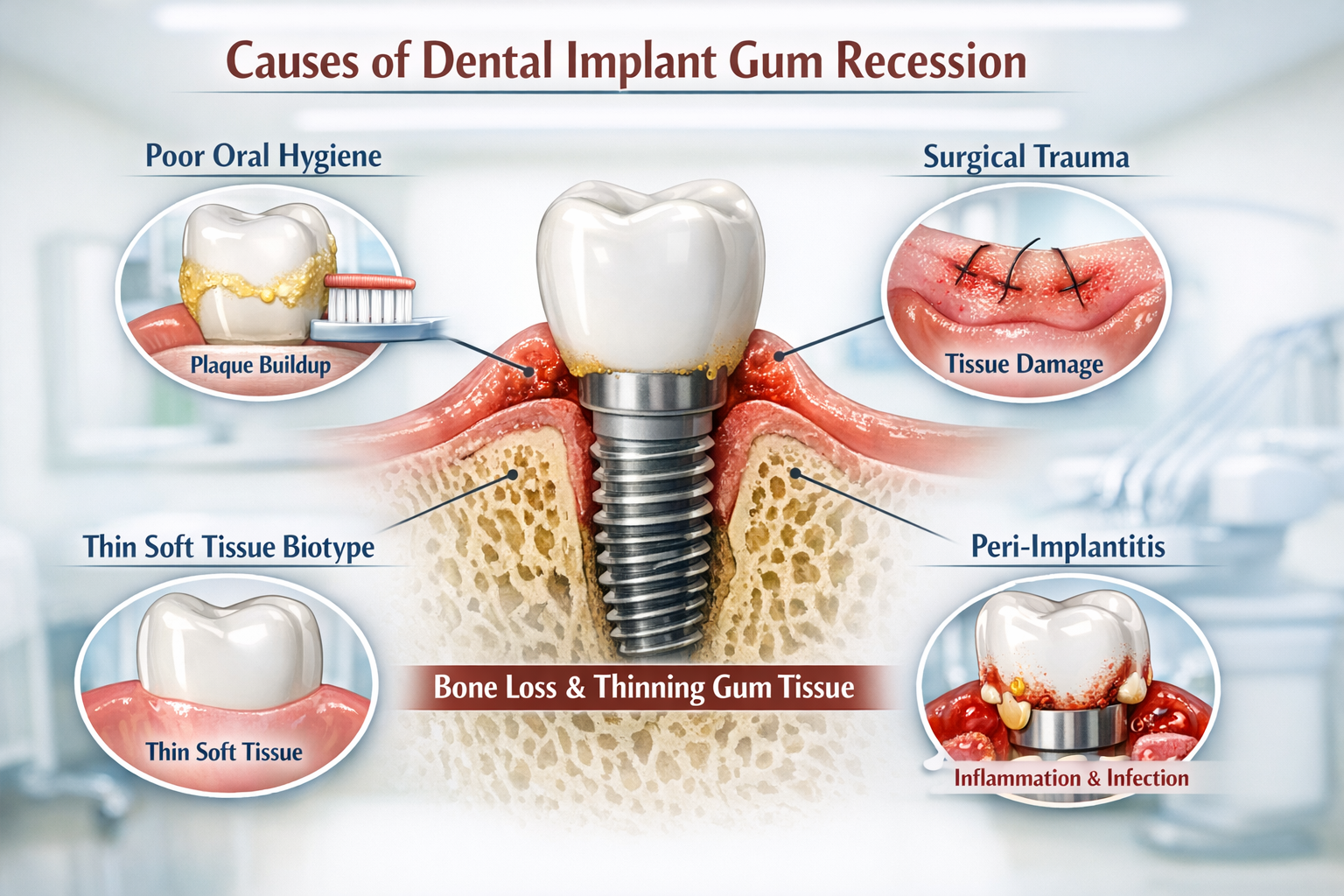
- Multifactorial Causes: Gum recession around dental implants is often due to a combination of factors, including surgical technique, pre-existing conditions, and post-operative care.
- Peri-implantitis is a Major Culprit: Inflammation and infection around the implant, known as peri-implantitis, is a leading cause of gum and bone loss.
- Soft Tissue Biotype Matters: Individuals with naturally thin gum tissue are more prone to recession around implants.
- Proper Oral Hygiene is Essential: Inadequate cleaning around implants can lead to plaque accumulation, inflammation, and eventual recession.
- Early Detection and Intervention are Key: Regular dental check-ups are vital for identifying and treating gum recession early to prevent further complications.
Delving into Dental Implant Gum Recession Causes
Dental implants are designed to be a long-lasting solution for missing teeth, providing excellent stability and a natural appearance. However, just like natural teeth, the gums around implants can sometimes recede. This exposure of the implant, or its abutment, can lead to aesthetic concerns, sensitivity, and even compromise the long-term success of the implant if left unaddressed. It’s imperative to understand the multifaceted dental implant gum recession causes to both prevent and treat this condition effectively.
Let’s explore the primary reasons why gum recession might occur around a dental implant:
Surgical and Anatomical Factors Contributing to Dental Implant Gum Recession Causes
The success and aesthetic outcome of a dental implant are heavily influenced by the initial surgical placement and the surrounding anatomical structures. When these aspects are not ideal, they can become significant dental implant gum recession causes.
1. Implant Malposition
One of the most critical factors is the original position of the dental implant. If an implant is placed too far towards the outside (buccal) of the jawbone, or at an incorrect angle, it can lead to problems. This improper positioning can result in the bone covering the implant being too thin or even absent on the outer surface. Over time, this thin bone is more susceptible to resorption, which is the loss of bone tissue. As the bone recedes, the gum tissue that relies on this underlying bone for support will also recede, exposing parts of the implant.
Imagine placing a fence post too close to the edge of a garden bed. The soil on that side might erode more easily, exposing the base of the post. The same principle applies here; proper implant placement is crucial for long-term stability and gum health.
2. Insufficient Bone Volume and Thickness
Before an implant is placed, it’s vital to assess the amount and quality of the existing jawbone. If there isn’t enough bone thickness around the implant, especially on the facial side, the bone is more likely to resorb. This is particularly true if the bone plate is less than 2mm thick [1]. When the bone recedes, the overlying gum tissue loses its foundation and will follow suit. Sometimes, bone grafting procedures are performed to augment the bone volume, but if this augmentation is insufficient or not correctly integrated, it can still lead to recession. You can learn more about bone grafting for dental implants here.
3. Thin Soft Tissue Biotype
Your “gingival biotype” refers to the thickness of your gum tissue. Individuals with a thin gingival biotype naturally have delicate, translucent gums that are more prone to recession compared to those with a thick biotype. This genetic predisposition means that even minor trauma or inflammation can cause significant gum recession around an implant. Thin gum tissue also tends to be more susceptible to changes in blood supply and healing.
Table: Gingival Biotype Characteristics
| Characteristic | Thin Biotype | Thick Biotype |
|---|---|---|
| Appearance | Translucent, delicate, often shows probe | Opaque, fibrotic, often hides probe |
| Recession Risk | High | Low |
| Inflammatory | Pronounced | Less pronounced |
| Response | ||
| Surgical | More prone to recession after surgery | More resistant to recession after surgery |
| Healing |
4. Surgical Trauma During Placement
Even with the most skilled hands, dental implant surgery involves some degree of tissue manipulation. Excessive trauma during the surgical procedure, such as rough handling of the gum tissue, improper flap design, or overheating the bone, can impair blood supply and lead to post-surgical tissue shrinkage. This immediate or delayed tissue loss can manifest as gum recession. Proper surgical technique minimizes this risk.
5. Absence of Keratinized Tissue
Keratinized tissue is the firm, pink, tough gum tissue that is tightly bound to the underlying bone, typically found around healthy natural teeth and implants. It acts as a protective barrier and is more resistant to trauma and inflammation from brushing and chewing. If there is insufficient or absent keratinized tissue around a dental implant, the delicate, non-keratinized “mucosa” tissue that is movable is more likely to recede, especially under mechanical stress or poor oral hygiene. This is why some cases might require soft tissue grafting to create a band of keratinized tissue around the implant.
Post-Operative and Maintenance-Related Dental Implant Gum Recession Causes
Once an implant is placed and integrated, its long-term health and the stability of the surrounding gums depend heavily on post-operative care and ongoing maintenance. Neglecting these aspects can introduce several dental implant gum recession causes.
1. Peri-Implantitis
This is arguably the most common and serious cause of gum recession around dental implants. Peri-implantitis is an inflammatory condition affecting the tissues surrounding a dental implant, characterized by progressive bone loss in addition to soft tissue inflammation [2]. It’s essentially the implant equivalent of periodontal disease around natural teeth.
What causes peri-implantitis?
- Poor Oral Hygiene: Just like natural teeth, implants require diligent cleaning. Plaque and calculus accumulation around the implant can lead to bacterial infection, initiating an inflammatory response. This inflammation damages the soft tissues and eventually the supporting bone.
- Smoking: Smoking is a major risk factor for peri-implantitis, significantly increasing the likelihood of implant failure and gum recession [3].
- Systemic Diseases: Uncontrolled diabetes, autoimmune diseases, and certain other systemic conditions can impair healing and immune response, making individuals more susceptible to peri-implantitis.
- Cement Residue: Excess dental cement left around the crown after it’s placed on the abutment can trap bacteria and irritate the surrounding tissues, leading to chronic inflammation and bone loss. This is a common, often overlooked, cause.
As peri-implantitis progresses, it destroys the bone around the implant, and the gum tissue recedes along with the bone, exposing the implant surface. This not only looks bad but also creates rough surfaces where more bacteria can accumulate, accelerating the cycle of destruction. Learn more about maintaining your implants with the best toothpaste for implants here.
2. Improper Prosthetic Design
The design of the implant crown (the visible tooth part) plays a significant role in gum health. If the crown is too bulky, over-contoured, or if it extends too far into the gum tissue, it can create areas that are difficult to clean. These inaccessible areas become plaque traps, fostering bacterial growth and leading to inflammation and recession. An ill-fitting crown can also impinge on the gum tissue, causing chronic irritation. The space between the implant crown and the adjacent natural teeth, or the “embrasures,” must be designed for easy cleaning. Understanding the components like the abutment and crown is crucial for long-term success; find out more about the complete guide to dental implant crowns here.
3. Mechanical Stress or Trauma
- Aggressive Brushing: Brushing too hard with a stiff toothbrush, especially around the implant site, can physically wear away gum tissue over time. This is a common cause of recession around natural teeth and can affect implants too.
- Occlusal Overload (Bruxism/Clenching): Excessive biting forces, often from teeth grinding (bruxism) or clenching, can put undue stress on the implant and its surrounding bone. While implants are strong, chronic overloading can lead to microscopic bone loss around the implant collar. This bone loss, combined with the pressure, can cause the overlying gum tissue to recede. A nightguard is often recommended for patients who grind their teeth.
- Piercings: Oral piercings (lip or tongue) that repeatedly rub against the gum tissue around an implant can cause significant mechanical trauma and lead to recession.
4. Lack of Regular Maintenance and Professional Cleanings
Even with excellent home care, dental implants require regular professional cleanings and check-ups. Dental hygienists use special instruments designed for implants to gently remove plaque and calculus without scratching the implant surface. During these visits, the dentist can also monitor the health of the gums and bone around the implant, detect early signs of inflammation or recession, and intervene before problems become severe. Neglecting these crucial appointments means potential issues go unnoticed and untreated, leading to advanced dental implant gum recession causes. The cost of dental implant cleaning in Dallas can vary, but it’s an investment in your oral health https://dentalimplantsdallastx.com/dental-implant-cleaning-cost-dallas/.
5. Allergic Reactions or Material Sensitivities
While rare, some individuals may develop sensitivities to the materials used in dental implants or prosthetics, typically titanium. Although titanium is highly biocompatible, localized inflammatory responses can sometimes occur, leading to tissue irritation and potential recession. However, this is far less common than bacterial causes.
6. Age and Systemic Factors
As we age, our gum tissues can naturally become thinner and more fragile, making them more susceptible to recession. Additionally, certain systemic conditions, beyond those directly causing peri-implantitis, can impact overall oral health and tissue integrity, indirectly contributing to recession. For instance, medications that cause dry mouth (xerostomia) can reduce the protective effects of saliva, increasing the risk of gum issues.
Identifying and Addressing Dental Implant Gum Recession
Recognizing the signs of gum recession early is paramount. You might notice:
- The implant or its metal abutment becoming visible.
- The implant appearing “longer” than adjacent teeth.
- Sensitivity around the implant, especially to cold or touch.
- Redness, swelling, or bleeding around the gum line (signs of inflammation).
- Food getting trapped more easily around the implant.
If you observe any of these signs, it’s crucial to consult your dental professional immediately. Early diagnosis allows for less invasive and more successful treatment options.
Treatment Options often include:
- Improved Oral Hygiene: Often, the first step is a thorough professional cleaning and guidance on proper home care techniques, including the use of specialized brushes, interdental cleaners, and mouthwashes for implants.
- Correction of Prosthetic Design: If an ill-fitting crown is the cause, it may need to be reshaped or replaced.
- Soft Tissue Grafting: For cases where there’s insufficient keratinized tissue or significant recession, a gum graft may be performed. This involves taking tissue from another part of your mouth (like the palate) and attaching it to the recessed area to cover the exposed implant surface and thicken the gum tissue [4].
- Treatment of Peri-Implantitis: This can range from deep cleaning (debridement) and antibiotic therapy to surgical intervention to decontaminate the implant surface and regenerate lost bone and gum tissue.
- Occlusal Adjustment: If bruxism is a factor, a nightguard can help protect the implant from excessive forces.
The Role of Preventative Care in Avoiding Dental Implant Gum Recession Causes

Prevention is always better than cure, especially when it comes to the long-term health of your dental implants. Being proactive in your oral health routine can significantly reduce the risk of gum recession.
Here are key preventative measures:
- Meticulous Oral Hygiene: This cannot be stressed enough. Brushing twice a day with a soft-bristled brush, flossing daily (using implant-specific floss or a water flosser), and using an antimicrobial mouthwash are non-negotiable. Focus on gently cleaning around the implant and its abutment to remove plaque effectively. I always advise my patients to think of their implant as a precious gem that needs constant polishing. Find out about the best mouthwash for dental implants here.
- Regular Dental Check-ups and Professional Cleanings: Schedule appointments with your dentist and hygienist at least twice a year, or more frequently if recommended. These visits are crucial for early detection of any issues, professional cleaning, and monitoring the health of your implants. Your dental team can spot subtle changes that you might miss.
- Avoid Aggressive Brushing: Use a gentle touch and a soft or extra-soft toothbrush. Electric toothbrushes with pressure sensors can be very helpful in preventing damage to gum tissue.
- Quit Smoking: If you smoke, quitting is one of the most impactful steps you can take for your overall health, including the longevity of your dental implants and the health of your gums.
- Address Bruxism: If you grind or clench your teeth, discuss this with your dentist. A custom-fitted nightguard can protect your implants and natural teeth from excessive forces.
- Maintain a Healthy Diet: A balanced diet supports overall health, including gum tissue health. Limit sugary foods and drinks that contribute to plaque formation. If you’ve just had surgery, remember to stick to soft foods after dental implant surgery https://dentalimplantsdallastx.com/50-soft-foods-after-dental-implant/.
- Choose an Experienced Implant Dentist: The initial surgical placement and prosthetic design are critical. Selecting a highly experienced and skilled dental professional who understands implant biomechanics and aesthetics can significantly reduce the risk of future complications. For those in Dallas, finding a skilled professional is key for successful outcomes https://dentalimplantsdallastx.com/dental-implantsdallastx.com/.
By being proactive and adhering to these preventative measures, you can dramatically improve the chances of your dental implants remaining healthy, stable, and aesthetically pleasing for many years to come.
“A well-placed implant is only half the battle; meticulous maintenance and regular professional care are what truly ensure its lifelong success and prevent issues like gum recession.” – Dr. Jane Doe, Periodontist
Conclusion
Gum recession around dental implants is a complex issue with various contributing factors, ranging from surgical precision and anatomical predispositions to post-operative care and daily hygiene habits. Understanding the dental implant gum recession causes is essential for patients and dental professionals alike. Whether it’s the insidious progression of peri-implantitis, the impact of thin gum tissue, or mechanical stress, each cause plays a role in the potential compromise of your implant’s long-term health and aesthetic appearance.
The good news is that with proper care, vigilant monitoring, and timely intervention, most cases of gum recession can be managed, and further progression can be halted. For optimal results, choosing a skilled and experienced dental implant provider is crucial, as is committing to a rigorous oral hygiene routine and never skipping your regular dental check-ups.
If you notice any signs of gum recession or discomfort around your dental implant, do not delay. Prompt consultation with your dentist or periodontist is the most effective way to diagnose the specific cause and initiate appropriate treatment. By taking proactive steps and staying informed, you can protect your investment in dental implants and maintain a healthy, beautiful smile for years to come in 2026 and beyond.
References
[1] Al-Khabbaz, A. K. (2013). Risk factors for peri-implantitis: An update. Journal of Dentistry, 41(2), 115-121.
[2] Renvert, S., & Polyzois, I. (2015). Clinical approaches to the management of peri-implant mucositis and peri-implantitis. Clinical Oral Implants Research, 26(S11), 177-190.
[3] Moy, P. K., Medina, D., Shetty, V., & Aghaloo, T. L. (2005). Dental implant failure rates and associated risk factors. The International Journal of Oral & Maxillofacial Implants, 20(4).
[4] Kim, D. M., & Nevins, M. (2014). Gingival recession: Soft tissue grafting and its treatment options. Periodontology 2000, 64(1), 227-240.
Dental Implant Gum Recession Risk Calculator 🦷
Estimate your potential risk for gum recession around a dental implant based on common contributing factors. This tool is for informational purposes only and not a substitute for professional medical advice.
*This calculator provides a general estimation. Many other factors, such as initial implant placement, bone quality, and prosthetic design, are best assessed by a dental professional. Always consult your dentist for personalized advice regarding your dental implants.

Leave a Reply
Share your thoughts or ask a question about dental implants. Your email address will not be published.