Imagine finally achieving that perfect smile and chewing comfort with dental implants, only to experience unexpected pain or discomfort years down the line. It can be concerning, even alarming. While dental implants boast an impressive success rate and are designed for long-term durability, it’s not uncommon for some individuals to experience dental implant discomfort years later. This comprehensive guide will delve into the various reasons why this discomfort might occur, what symptoms to look out for, and the effective solutions available to restore your oral health and peace of mind. As an expert SEO content strategist and senior editor, my goal is to provide you with high-authority information to navigate this potential challenge.
Key Takeaways
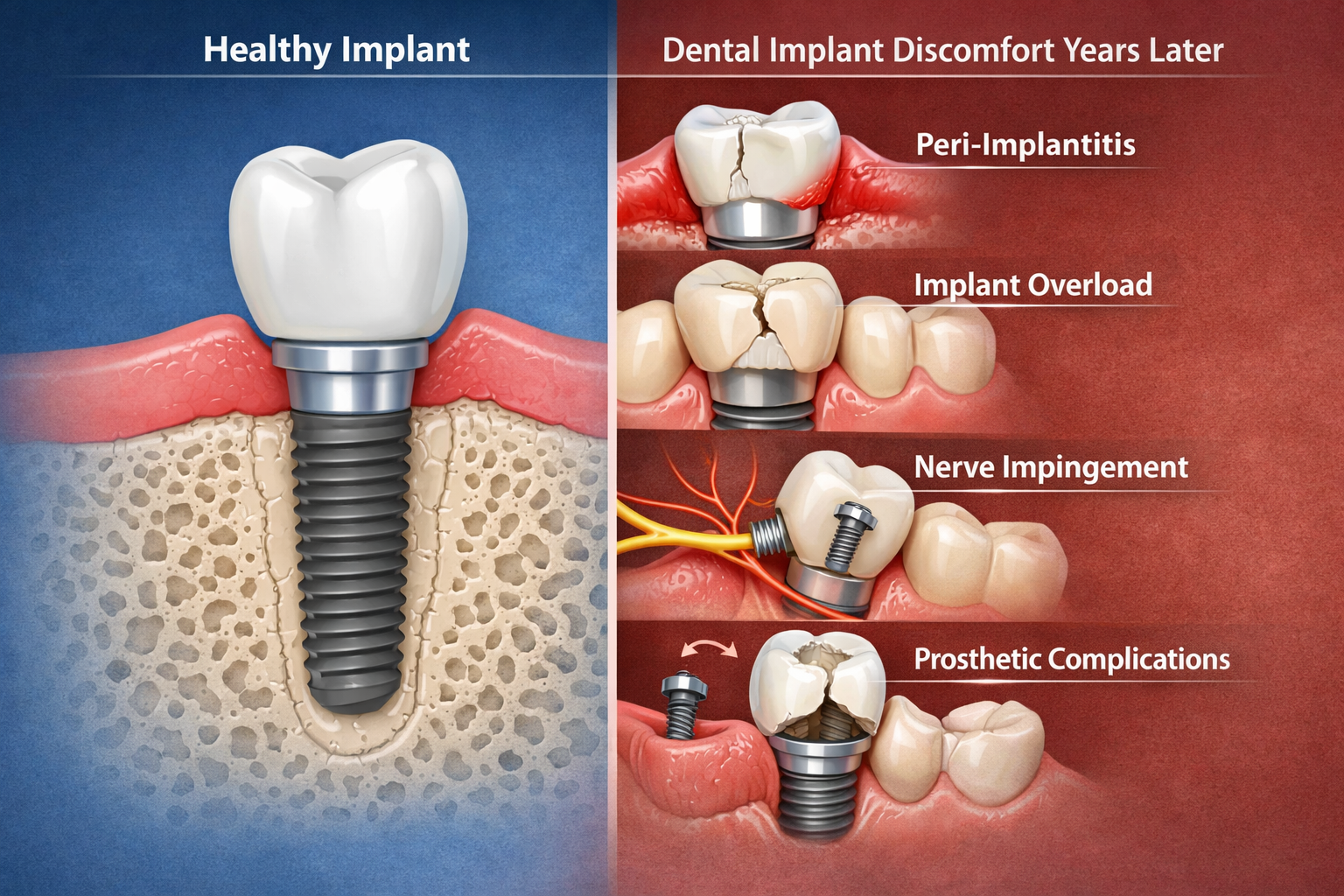
- Dental implant discomfort years later can stem from various causes, including biological factors like peri-implantitis, mechanical issues with the implant components, or nerve impingement.
- Symptoms range from mild throbbing and swelling to severe pain, loose crowns, or visible changes in gum tissue around the implant.
- Early detection and prompt dental consultation are crucial for effective treatment and preventing more severe complications.
- Treatment options vary widely based on the underlying cause and can include deep cleaning, antibiotics, bone grafting, prosthetic adjustments, or in rare cases, implant removal.
- Maintaining excellent oral hygiene and regular dental check-ups are paramount for the long-term success and comfort of your dental implants.
Why Does Dental Implant Discomfort Years Later Occur?
Dental implants are a significant investment in your oral health, offering a permanent and stable solution for missing teeth. They are designed to mimic natural tooth roots, integrating with your jawbone through a process called osseointegration. However, even with meticulous care and successful initial healing, issues can sometimes arise, leading to dental implant discomfort years later. Understanding these potential causes is the first step toward effective management.
Biological Factors Contributing to Discomfort
The most common biological reasons for late-onset dental implant discomfort often involve the soft and hard tissues surrounding the implant.
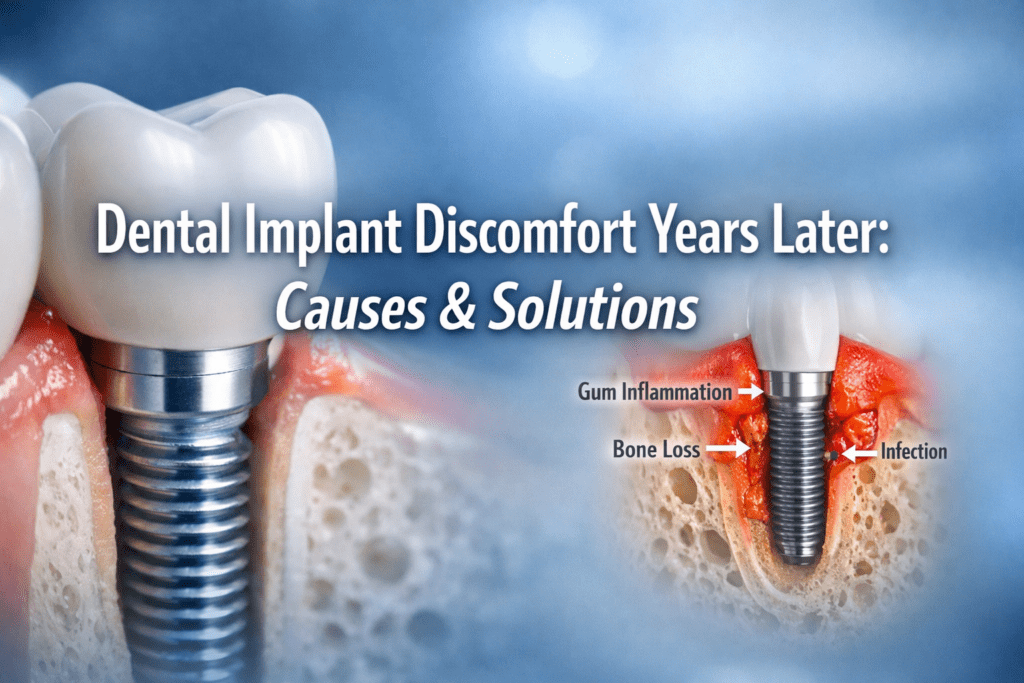
1. Peri-Implantitis
Peri-implantitis is arguably the most significant biological complication associated with dental implants and a primary cause of dental implant discomfort years later. It’s a chronic inflammatory disease affecting the soft tissues and bone supporting the implant, essentially similar to periodontal disease around natural teeth [1].
What happens:
- Bacterial accumulation: Plaque and bacteria build up around the implant, often due to inadequate oral hygiene.
- Inflammation: This leads to inflammation of the gum tissue (peri-implant mucositis), which, if left untreated, progresses to affect the supporting bone.
- Bone loss: As the disease advances, it causes progressive destruction of the bone around the implant, leading to reduced support and potentially implant mobility.
Symptoms of Peri-Implantitis:
- Red, swollen, or bleeding gums around the implant.
- Pus discharge.
- Persistent bad taste or bad breath.
- Deepening of the peri-implant pocket (the space between the gum and the implant).
- Radiographic bone loss visible on X-rays.
- Dull ache or throbbing pain, especially when chewing.
- In advanced stages, the implant may feel loose.
Timely intervention is critical for peri-implantitis. If you notice any of these symptoms, don’t delay. A visit to your dentist or periodontist is essential to assess the situation and initiate appropriate treatment. You can learn more about specialized care at dallas periodontics dental implants.
2. Insufficient Osseointegration (Late Failure)
While most implant failures due to poor osseointegration occur early in the healing process, sometimes an implant that initially appeared stable can lose its bone integration years later. This is less common but can be a cause of discomfort.
Causes:
- Systemic health changes: Conditions like uncontrolled diabetes, osteoporosis, or certain medications (e.g., bisphosphonates) can impact bone metabolism.
- Excessive occlusal load: Constant, heavy biting forces or grinding (bruxism) can overload the implant, leading to stress fractures in the surrounding bone or the implant itself, compromising osseointegration.
- Poor bone quality/quantity: While typically assessed before placement, subtle bone degradation over time can contribute.
Symptoms might include persistent pain, a feeling of looseness in the implant crown, or even the implant itself.
3. Nerve Impingement
In rare cases, if an implant is placed too close to a nerve canal, it can cause nerve damage or compression. While acute nerve damage usually manifests immediately after surgery, chronic pressure or inflammation years later could lead to symptoms. This is more common with implants in the lower jaw, near the inferior alveolar nerve.
Symptoms:
- Numbness or tingling (paresthesia) in the lip, chin, or tongue on the affected side.
- Persistent pain, which may be burning or shooting in nature.
- Altered sensation.
Mechanical and Prosthetic Complications
Beyond biological issues, the components that make up the implant system can also be a source of discomfort.
1. Loose or Fractured Components
The dental implant system consists of three main parts: the implant fixture (in the bone), the abutment (connecting the fixture to the crown), and the crown (the visible tooth). Any of these can develop issues.
- Loose abutment screw: The screw connecting the abutment to the implant fixture can loosen over time due to chewing forces. This often presents as a subtle clicking sound, a feeling of movement, or mild discomfort when chewing.
- Loose or fractured crown: The crown itself can become loose from the abutment, or it can fracture due to excessive force or wear. This can lead to pain, sensitivity, or food impaction. If you’re experiencing a loose or fractured crown, it might be related to the abutment supported porcelain ceramic crown component of your implant.
- Fractured implant fixture: While rare due to the strength of titanium, an implant fixture can fracture under extreme, long-term stress, especially in cases of severe bruxism or poor initial bone integration. This is a serious complication requiring specialist intervention.
2. Ill-fitting Prosthesis
If the implant crown or bridge doesn’t fit perfectly, it can create problems.
- Uneven bite (occlusal discrepancies): An implant crown that is too high or improperly aligned can put excessive force on the implant, the surrounding bone, or even opposing teeth. This can lead to localized pain, jaw pain, or even headaches.
- Food impaction: Gaps between the implant crown and adjacent teeth can allow food particles to get stuck, leading to gum irritation, inflammation, and discomfort.
- Poor contour: An improperly shaped crown can make cleaning difficult, contributing to plaque buildup and peri-implantitis.
3. Adjacent Tooth Issues
Sometimes, the discomfort isn’t directly from the implant but from a neighboring tooth or structure.
- Decay or fracture in an adjacent tooth: Pain from an adjacent tooth can be misattributed to the implant.
- Periodontal disease in adjacent teeth: If surrounding natural teeth develop gum disease, it can affect the overall oral environment and potentially spread to the implant.
- TMJ (Temporomandibular Joint) disorders: Jaw pain or muscle soreness from TMJ issues can sometimes be perceived as originating from the implant area.
Recognizing the Symptoms: When to Seek Help for Dental Implant Discomfort Years Later
Identifying the signs of dental implant discomfort years later is crucial for prompt diagnosis and treatment. Don’t wait for the pain to become unbearable.
Common Symptoms to Monitor:
| Symptom Category | Specific Manifestations | Potential Underlying Cause |
|---|---|---|
| Pain & Discomfort | Dull ache, throbbing pain, sharp pain when biting, persistent soreness, burning sensation. | Peri-implantitis, nerve impingement, mechanical issues, occlusal overload. |
| Swelling & Redness | Gums around the implant appear swollen, puffy, or unusually red. | Peri-implantitis, infection. |
| Bleeding | Gums bleed easily when brushing or flossing around the implant. | Peri-implantitis, peri-implant mucositis. |
| Pus Discharge | Visible pus exudate from the gum margin around the implant. | Active infection, advanced peri-implantitis. |
| Loose Feeling | The implant crown feels loose, or you sense movement in the implant itself. | Loose screw, loose crown, loss of osseointegration, fractured implant. |
| Clicking/Grinding | Audible clicking or grinding sounds from the implant area when chewing. | Loose abutment screw, prosthetic component issues. |
| Bad Taste/Breath | Persistent metallic taste, bad breath that doesn’t resolve with hygiene. | Bacterial infection, peri-implantitis. |
| Gum Recession | Gums around the implant recede, exposing parts of the implant or abutment. | Peri-implantitis, trauma, poor implant placement. |
| Numbness/Tingling | Persistent numbness or altered sensation in the lip, chin, or tongue. | Nerve impingement (more common with lower jaw implants). |
💬 “Any persistent discomfort or changes around your dental implant, no matter how minor, warrants immediate attention from your dentist. Early intervention can prevent minor issues from escalating into major complications.”
Diagnosing the Cause of Dental Implant Discomfort Years Later
When you visit your dentist with concerns about dental implant discomfort years later, they will conduct a thorough examination to pinpoint the cause.
Diagnostic Steps:
- Clinical Examination:
- Visual inspection: Checking for redness, swelling, pus, gum recession.
- Probing: Gently measuring the pocket depth around the implant to assess gum health.
- Mobility testing: Gently checking if the implant or crown is loose.
- Occlusal assessment: Evaluating your bite to ensure the implant crown is not under excessive force.
- Radiographic Evaluation (X-rays and CT Scans):
- Periapical X-rays: To visualize bone levels around the implant and detect any bone loss.
- Panoramic X-rays: To get a broader view of your jaw and identify potential nerve proximity issues.
- CBCT (Cone Beam Computed Tomography) scan: Provides a detailed 3D image, invaluable for assessing bone quality, nerve pathways, and identifying fractures that might not be visible on 2D X-rays. Learn more about CT scans and dental implants.
- Bacterial Sampling: In cases of suspected infection, a sample of bacteria from around the implant may be taken to identify specific pathogens and guide antibiotic therapy.
Treatment Options for Dental Implant Discomfort Years Later

The treatment for dental implant discomfort years later is highly dependent on the underlying cause. Your dentist will tailor a treatment plan specific to your situation.
1. Addressing Peri-Implantitis
- Non-Surgical Debridement: For early-stage peri-implantitis (peri-implant mucositis), professional cleaning to remove plaque and calculus from around the implant surface, often combined with antimicrobial rinses or localized antibiotics.
- Surgical Interventions:
- Open flap debridement: Lifting the gum tissue to thoroughly clean the implant surface and remove diseased tissue.
- Implant surface decontamination: Various methods (mechanical, laser, chemical) to remove bacteria and toxins from the implant surface.
- Bone grafting: If significant bone loss has occurred, a bone graft recovery dental implant procedure may be performed to regenerate lost bone around the implant, improving its support and prognosis. This is often done in conjunction with guided tissue regeneration.
- Systemic Antibiotics: May be prescribed in conjunction with local treatments for active infections.
2. Resolving Mechanical and Prosthetic Issues
- Tightening Loose Screws: A simple and common fix for a loose abutment screw. The crown is removed, the screw is tightened to the correct torque, and the crown is re-cemented or re-attached.
- Prosthetic Repair or Replacement:
- Crown repair/replacement: If the crown is chipped, fractured, or ill-fitting, it can be repaired or replaced.
- Abutment replacement: If the abutment itself is damaged or causing issues, it can be replaced. Understanding the complete guide to the dental implant abutment procedure can provide further insights.
- Occlusal Adjustment: Carefully adjusting the biting surface of the implant crown to ensure even force distribution and eliminate “high spots” that cause discomfort or overload. This is critical for preventing future mechanical issues.
- Nightguard Fabrication: For patients with bruxism (teeth grinding or clenching), a custom nightguard can protect the implant and natural teeth from excessive forces.
3. Managing Nerve Impingement
- Conservative Management: For mild, transient symptoms, watchful waiting and pain management may be recommended.
- Surgical Intervention: In severe cases of persistent pain or numbness, surgical removal of the implant may be necessary to relieve pressure on the nerve. This is a last resort and requires careful consideration.
4. Implant Removal (Explantation)
In rare and severe cases where an implant is severely infected, fractured beyond repair, or has completely lost its bone integration, removal of the implant (explantation) may be the only viable option. After explantation, the site may be allowed to heal, and a new implant may be placed after a period of recovery, potentially with bone grafting to rebuild the site.
Prevention is Key: Ensuring Long-Term Implant Success
While treatment options exist for dental implant discomfort years later, prevention is always the best approach. Proactive care significantly increases the longevity and comfort of your implants.
Essential Practices for Implant Care:
- Impeccable Oral Hygiene:
- Brush twice daily: Use a soft-bristled toothbrush or an electric toothbrush, paying special attention to the gumline around implants.
- Floss daily: Use dental floss, interdental brushes, or a water flosser (like the best water flosser for dental implants) to clean around implants and between teeth.
- Use appropriate toothpaste and mouthwash: Your dentist can recommend the best toothpaste for implants and best mouthwash for dental implants.
- Regular Dental Check-ups:
- Professional cleanings: Schedule appointments every 6 months, or more frequently if recommended by your dentist, for specialized cleaning around implants.
- Comprehensive examinations: Your dentist will monitor your implants, surrounding tissues, and overall oral health.
- Radiographic monitoring: Periodic X-rays help detect bone changes around implants early.
- Avoid Harmful Habits:
- Smoking: Tobacco significantly increases the risk of peri-implantitis and implant failure.
- Excessive alcohol consumption: Can impair healing and overall oral health.
- Chewing hard foods: Avoid biting down on ice, hard candies, or other extremely hard objects that can damage implant crowns or even the implants themselves.
- Manage Systemic Health:
- Control chronic diseases: Conditions like diabetes can impact implant success. Work with your physician to keep systemic health conditions well-managed.
- Communicate medications: Inform your dentist about all medications you are taking, as some can affect bone health or healing.
- Address Bruxism: If you grind or clench your teeth, discuss it with your dentist. A nightguard can protect your implants and natural teeth from excessive forces.
By adhering to these preventive measures, you are taking active steps to ensure the long-term health and comfort of your dental implants, allowing them to serve you effectively for many years. For more guidance on post-operative care, explore our complete dental implant recovery timeline.
Conclusion
Experiencing dental implant discomfort years later can be unsettling, but it’s important to remember that most issues are treatable, especially when caught early. Dental implants are a highly successful and durable solution for tooth replacement, but they are not immune to problems. Whether the discomfort stems from biological factors like peri-implantitis, mechanical issues with the components, or even problems with adjacent teeth, understanding the potential causes is the first step toward effective resolution.
If you are experiencing any form of pain, swelling, redness, or a loose feeling around your dental implant, do not hesitate to contact your dental professional immediately. A thorough examination, including clinical assessment and radiographic imaging, will help determine the exact cause of your discomfort. From non-surgical cleanings and medication to prosthetic adjustments or, in rare cases, surgical intervention, your dentist will recommend the most appropriate treatment plan to restore your comfort and protect your investment.
Remember, prevention through diligent oral hygiene, regular dental check-ups, and a healthy lifestyle remains the cornerstone of long-term dental implant success. By being proactive and responsive to any changes in your oral health, you can ensure your dental implants continue to provide a confident smile and comfortable chewing for decades to come.
References
[1] Albrektsson, T., & Isidor, F. (1994). Consensus report of Session IV. European Journal of Oral Sciences, 102(Suppl 1), 606-608.
Dental Implant Discomfort Symptom Checker
Select the symptoms you are experiencing with your dental implant to get an idea of potential causes and what steps to take next. This tool is for informational purposes only and not a substitute for professional dental advice.

Leave a Reply
Share your thoughts or ask a question about dental implants. Your email address will not be published.