Undergoing a dental implant procedure is a significant step towards restoring your smile and oral health. It’s a highly effective solution for missing teeth, offering durability and a natural appearance. However, as with any surgical procedure, there’s a recovery period, and it’s natural to have questions and concerns about what to expect. One common observation that can cause alarm is spitting blood after dental implant surgery. Is it normal? When should you be worried? As an expert SEO content strategist and senior editor, I’m here to provide a comprehensive, high-authority guide to help you understand this aspect of your recovery in 2026.
Dental implant surgery involves placing a titanium post into your jawbone, which then integrates with the bone over several months. This process, known as osseointegration, is crucial for the implant’s stability. Given the nature of this procedure, some degree of bleeding is almost always expected. But the amount and duration of bleeding are key indicators of whether your recovery is progressing normally or if there might be an issue that requires professional attention. My goal is to equip you with the knowledge to distinguish between minor, expected bleeding and signs that warrant a call to your dental professional.
Key Takeaways
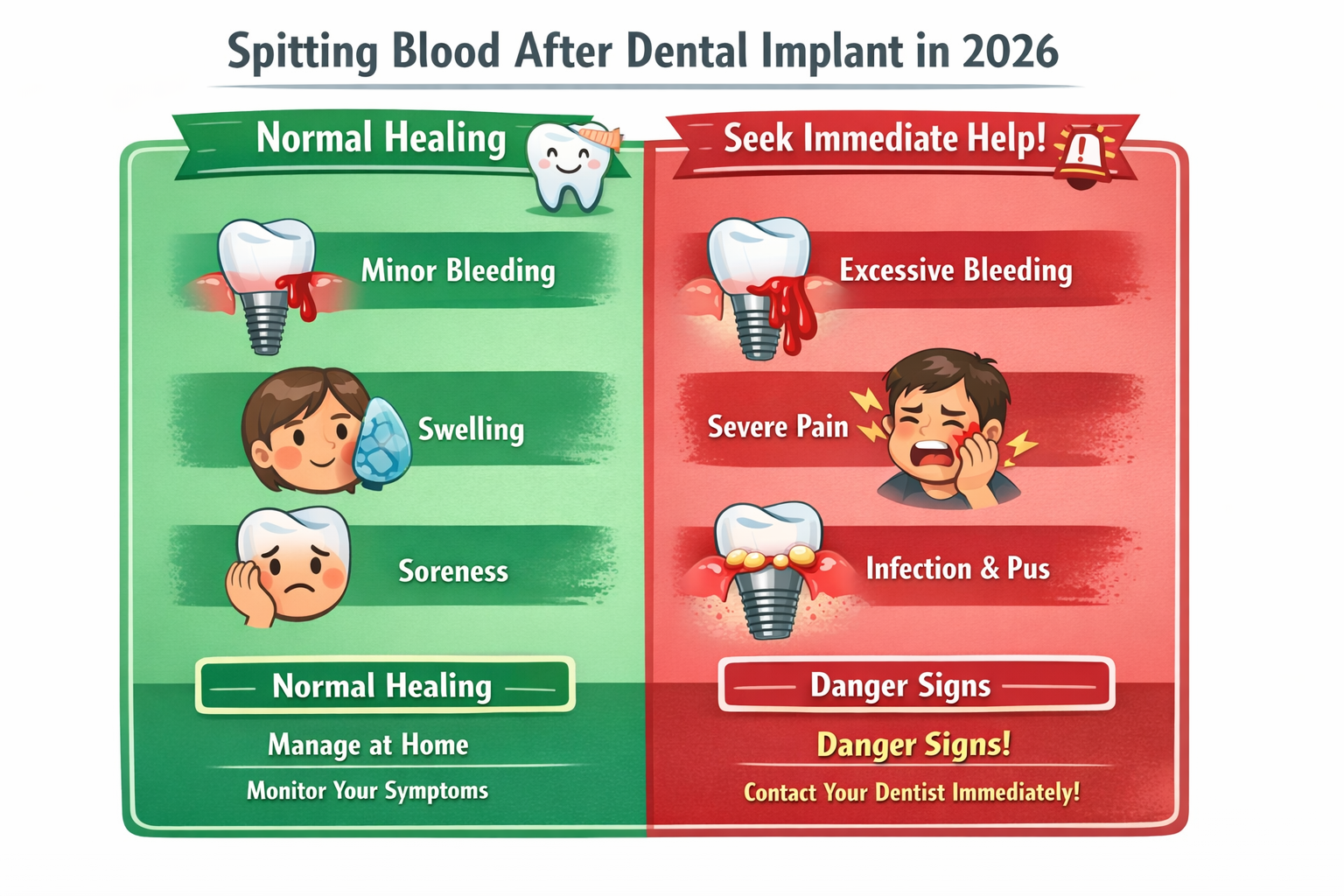
- Initial Bleeding is Normal: Light bleeding or a pinkish tint when spitting is common for the first 24-48 hours after dental implant surgery.
- Manage Bleeding Effectively: Applying pressure with gauze and avoiding activities that dislodge blood clots are crucial for controlling post-operative bleeding.
- Persistent or Excessive Bleeding is a Concern: If you are spitting blood after dental implant surgery for more than 48 hours, or if the bleeding is heavy and continuous, contact your dentist immediately.
- Follow Post-Operative Instructions: Adhering strictly to your dental professional’s aftercare instructions is the best way to ensure proper healing and minimize complications.
- Don’t Hesitate to Seek Advice: When in doubt, always reach out to your dental care provider for clarification or assessment.
Understanding Normal Bleeding After Dental Implant Surgery
It’s important to set realistic expectations about the recovery process. Dental implant placement is a surgical procedure that involves incisions in the gums and drilling into the jawbone. Therefore, experiencing some degree of bleeding afterward is not only normal but expected. Think of it like a minor cut or scrape; it will bleed a little before clotting.
What Constitutes “Normal” Bleeding?
For most patients, normal bleeding after dental implant surgery typically manifests as a slight oozing or a pinkish discoloration in your saliva when you spit. This usually occurs for the first 24 to 48 hours post-surgery. You might notice it more acutely when you wake up in the morning, as blood can accumulate overnight. This minor bleeding is often a sign that your body is beginning the natural healing process and forming a protective blood clot over the surgical site.
Table: Expected Bleeding After Dental Implant Surgery
| Timeframe After Surgery | Expected Bleeding Characteristics | Action Required |
|---|---|---|
| First 2-4 Hours | Moderate oozing, noticeable pink/red saliva. | Maintain pressure with gauze. |
| First 24-48 Hours | Light oozing, pinkish tint to saliva, occasional small clots. | Follow aftercare instructions, avoid rinsing vigorously. |
| Beyond 48 Hours | Very minimal or no bleeding. | Continue gentle oral hygiene. |
“A little bit of blood goes a long way in saliva, so what looks like a significant amount might just be a small ooze mixed with saliva. This is why understanding the characteristics of normal bleeding is crucial.”
It’s vital to differentiate between actual bleeding and saliva mixed with a small amount of blood. A few drops of blood can turn a significant amount of saliva red, making it appear more dramatic than it actually is. If you’re simply seeing a pink or light red tinge in your saliva, especially within the first day or two, it’s generally considered part of the normal healing process.
The Role of Blood Clots
Blood clots are your body’s natural bandages. After your dental implant is placed, a blood clot forms at the surgical site. This clot is crucial for two main reasons:
- Stops Bleeding: It acts as a plug to prevent further bleeding.
- Protects the Site: It protects the underlying bone and soft tissues from bacteria and irritation, initiating the healing cascade.
Dislodging this blood clot can lead to a condition called “dry socket” (though less common with implants than extractions) and can also prolong bleeding and delay healing. Therefore, careful management of the surgical site is paramount in the initial hours and days following your procedure. To learn more about proper aftercare, refer to our dental implant aftercare instructions.
Managing Post-Operative Bleeding
Proper management of post-operative bleeding is critical for comfortable recovery and successful implant integration. Your dental professional will provide specific instructions, but here are some general guidelines that apply to most situations when you are spitting blood after dental implant.
Immediate Steps After Surgery
After your dental implant surgery, your surgeon will likely place a sterile gauze pad over the surgical site and ask you to bite down firmly. This pressure is essential for helping a blood clot form.
- Maintain Pressure: Keep biting down on the gauze for at least 30-60 minutes. If the bleeding persists, you can replace the gauze with a fresh one and bite down again for another 30-60 minutes. Repeat this until the bleeding significantly subsides. Use moistened tea bags (black tea contains tannic acid, a natural coagulant) wrapped in gauze as an alternative if needed.
- Avoid Excessive Spitting or Rinsing: While it might feel counterintuitive when you are spitting blood after dental implant, try to avoid spitting or rinsing vigorously. This action can dislodge the crucial blood clot that is forming, leading to increased bleeding. If you need to clear your mouth, gently let the saliva drain or dab it with a tissue.
- Head Elevation: When resting or sleeping, keep your head elevated with an extra pillow. This can help reduce blood flow to the surgical site and minimize bleeding.
What to Avoid to Prevent Increased Bleeding
Certain activities and habits can interfere with clot formation and lead to increased or prolonged bleeding.
- Smoking: Smoking significantly impedes the healing process and increases the risk of complications, including bleeding and infection. It’s strongly advised to avoid smoking for at least several days, if not weeks, after your surgery.
- Alcohol: Alcohol can thin the blood and interfere with clotting. Avoid alcoholic beverages for at least 24-48 hours post-surgery. You can learn more about this on our page about alcohol after dental implant surgery.
- Hot Liquids and Foods: Extremely hot foods or beverages can increase blood flow to the surgical area and potentially dislodge clots. Stick to cool or lukewarm items.
- Strenuous Activity: Any vigorous physical activity can raise your blood pressure, which in turn can lead to increased bleeding at the surgical site. Take it easy for a few days after your procedure.
- Straws: The sucking motion used with straws creates negative pressure in the mouth, which can easily dislodge a blood clot. Avoid using straws for at least the first week.
By following these guidelines, you significantly increase your chances of a smooth and uneventful recovery, minimizing the issue of spitting blood after dental implant. For a detailed timeline of recovery, see our complete dental implant recovery timeline.
When Spitting Blood After Dental Implant Becomes a Concern

While some bleeding is normal, there are instances where the amount or duration of blood you’re spitting after a dental implant could indicate a problem. Knowing these warning signs is crucial for your safety and the success of your implant.
Signs of Abnormal Bleeding
You should contact your dental surgeon or oral healthcare provider immediately if you experience any of the following:
- Heavy, Continuous Bleeding: If the surgical site continues to bleed heavily (saturating gauze rapidly, constant flow of bright red blood) for more than a few hours, even after applying pressure, it’s a sign that something is amiss. This is more than just a pinkish tinge; it’s significant, uncontrolled bleeding.
- Bleeding Beyond 48 Hours: While a very slight pink tinge might linger for a bit longer, significant spitting blood after dental implant beyond 48 hours post-surgery is generally not normal. This could indicate a persistent vascular issue or a dislodged clot that hasn’t re-formed properly.
- Large Blood Clots: While small clots are normal, expelling large, jelly-like blood clots can be a sign that the primary clot at the surgical site is not stable.
- Unusual Pain or Swelling Accompanying Bleeding: While some pain and swelling are expected, if the bleeding is accompanied by severe, worsening pain that isn’t managed by prescribed medication, or if the swelling is rapidly increasing, this could signal an underlying complication like infection or an issue with the implant site.
Potential Causes of Excessive or Prolonged Bleeding
Several factors can contribute to abnormal bleeding. Understanding these can help you identify potential issues:
- Dislodged Blood Clot: As mentioned, vigorous rinsing, spitting, or trauma to the area can dislodge the protective blood clot, leading to renewed bleeding.
- Medication Interference: Certain medications, especially blood thinners (anticoagulants or antiplatelet drugs), can increase the risk of bleeding. It’s crucial to inform your surgeon about all medications you are taking, including over-the-counter drugs and supplements, before your surgery. Your surgeon might adjust your medication regimen temporarily.
- Underlying Health Conditions: Undiagnosed or poorly managed bleeding disorders can also lead to excessive post-operative bleeding. Again, a thorough medical history prior to surgery is vital.
- Surgical Site Trauma: Sometimes, accidental trauma to the surgical site (e.g., bumping it, hard chewing) can reopen the wound and cause bleeding.
- Infection: While less common in the immediate aftermath, an infection could sometimes manifest with bleeding, often accompanied by pain, swelling, and possibly pus or fever. Signs of infection usually appear a few days post-op rather than immediately.
- Bone Graft Complications: If a bone graft was performed alongside your implant, there might be slightly more bleeding, but it should still be manageable and not excessive. Issues with the graft site could lead to prolonged bleeding. Find out more about bone graft recovery for dental implants.
Remember: It is always better to be safe than sorry. If you are concerned about the amount or duration of bleeding, do not hesitate to contact your dental implant specialist or oral surgeon. They are the best resource for evaluating your situation and providing appropriate guidance. For complex cases, our team at dentalimplantsdallastx.com is always ready to assist.
The Importance of Following Post-Operative Instructions
The success of your dental implant and the smoothness of your recovery heavily depend on how diligently you follow your dental professional’s post-operative instructions. These instructions are tailored to minimize complications like excessive bleeding and infection and to promote optimal healing.
Key Post-Operative Care Guidelines
While specific instructions may vary slightly depending on your individual case and your surgeon’s preferences, some guidelines are universally applicable:
- Medication Management:
- Pain Relievers: Take prescribed pain medication as directed. Do not wait for the pain to become severe.
- Antibiotics: If prescribed, take the full course of antibiotics exactly as instructed. This is critical for preventing infection, which can complicate healing and potentially lead to bleeding. Learn more about antibiotics after dental implant surgery.
- Oral Hygiene:
- Gentle Rinsing: After the first 24 hours, you may be instructed to gently rinse your mouth with a warm salt water solution (1/2 teaspoon salt in 8 ounces of warm water) several times a day, especially after meals. This helps to keep the area clean and reduce bacteria. Remember, gentle rinsing – do not swish vigorously.
- Brushing: Be extremely careful when brushing your teeth, especially near the surgical site. Avoid direct brushing of the implant site for the first few days. Your dentist might recommend a very soft toothbrush or a specialized brush for the area.
- Dietary Modifications:
- Soft Foods: For the first few days (or longer, as advised), stick to a diet of soft, cool foods. This reduces trauma to the surgical site and prevents the dislodgement of blood clots. Think yogurt, mashed potatoes, soups (lukewarm), smoothies. For more ideas, check out our list of 50 soft foods after dental implant.
- Avoid Hard, Crunchy, or Sticky Foods: These foods can irritate the surgical site, become lodged in the wound, or put undue pressure on the implant.
- Rest: Get plenty of rest. Your body needs energy to heal. Avoid strenuous activities for at least the first 24-48 hours, or longer if advised.
The Impact of Neglecting Instructions
Ignoring these instructions can have several negative consequences:
- Increased Bleeding: As discussed, improper rinsing, dietary choices, or physical activity can disrupt blood clots and lead to prolonged or heavier bleeding.
- Infection: Poor oral hygiene or failure to take antibiotics can lead to bacterial infection, which not only causes pain and discomfort but can also jeopardize the success of your implant.
- Delayed Healing: Any complication, whether it’s infection or excessive bleeding, will inevitably slow down the overall healing process and the critical osseointegration period.
- Implant Failure: In severe cases, complications arising from neglected aftercare can lead to implant failure, requiring additional, costly procedures.
Your dental implant is a significant investment in your oral health. Treating the post-operative period with the seriousness it deserves by meticulously following all instructions is paramount to achieving the best possible outcome. If you have any questions about your specific instructions or concerns about your recovery, don’t hesitate to contact your dental professional at dentalimplantsdallastx.com/contact-us/.
Long-Term Considerations and Prevention
While this article primarily focuses on immediate post-operative bleeding, it’s also worth discussing long-term considerations that can affect your implant’s health and how to prevent future issues. Maintaining excellent oral hygiene and regular dental check-ups are paramount for the longevity of your dental implant.
Preventing Future Bleeding or Complications
Once the initial healing phase is complete, your focus shifts to long-term maintenance. Even years after your procedure, issues can arise, and preventing them is key.
- Maintain Excellent Oral Hygiene: This is non-negotiable. Treat your dental implant like your natural teeth, perhaps even better.
- Brushing: Brush at least twice a day with a soft-bristled toothbrush. Consider an electric toothbrush designed for implants.
- Flossing: Floss daily. Special implant-specific floss or interdental brushes may be recommended to clean around the implant abutment and crown.
- Mouthwash: Use a non-alcoholic antibacterial mouthwash if recommended by your dentist. Some patients benefit from a specialized best mouthwash for dental implants.
- Regular Dental Check-ups: Schedule regular check-ups and professional cleanings with your dentist. They can monitor the health of your implant, surrounding gums, and bone, catching potential issues early. Your cleaning might involve special tools designed not to scratch the implant surface. You can learn more about dental implant cleaning cost on our site.
- Avoid Harmful Habits:
- Smoking: Continue to avoid smoking. It dramatically increases the risk of peri-implantitis (gum disease around an implant) and implant failure.
- Hard Foods: While you can generally eat normally once your implant has fully integrated, avoid excessively hard foods that could damage the crown or abutment.
- Teeth Grinding/Clenching: If you grind or clench your teeth (bruxism), inform your dentist. They might recommend a nightguard to protect your implant and natural teeth from excessive force.
- Address Any Concerns Promptly: If you notice any redness, swelling, tenderness, or bleeding around your implant site, even months or years after placement, contact your dentist immediately. These could be early signs of peri-implantitis, an inflammatory condition that can lead to bone loss around the implant and potentially implant failure.
Peri-implantitis and Its Symptoms
Peri-implantitis is a serious inflammatory condition affecting the tissues surrounding a dental implant, leading to progressive bone loss. It’s similar to periodontal disease in natural teeth.
Common Symptoms of Peri-implantitis:
- Bleeding: Bleeding when brushing or flossing around the implant, or spontaneous bleeding. This can manifest as spitting blood.
- Redness and Swelling: Inflammation of the gum tissue around the implant.
- Pain or Tenderness: Discomfort around the implant, especially when chewing or touching the area.
- Pus: Discharge of pus from the gum line around the implant.
- Receding Gums: The gum tissue pulling away from the implant.
- Loose Implant: In advanced stages, the implant may become noticeably loose.
If diagnosed early, peri-implantitis can often be managed effectively, sometimes with non-surgical treatments or, in more advanced cases, with surgical intervention. Ignoring the symptoms, especially recurring bleeding or spitting blood after dental implant (even long after the initial healing), can lead to irreversible bone loss and eventual implant failure.
Maintaining open communication with your dental professional and being proactive about your oral health are your best defenses against long-term complications and ensure your dental implants last for many years to come. For more information on dental implants and their care, explore our main dental implants Dallas TX page.
Conclusion

Experiencing some degree of spitting blood after dental implant surgery is a common and usually normal part of the healing process. For the first 24 to 48 hours, a pinkish tinge in your saliva or slight oozing from the surgical site is generally no cause for alarm. This is your body’s natural response as it forms the crucial blood clot necessary for healing and ultimately, the successful integration of your new dental implant.
However, understanding when this normal bleeding crosses into a concerning territory is vital. Persistent, heavy bleeding that saturates gauze quickly, or any significant bleeding that continues beyond 48 hours, warrants immediate attention from your dental professional. Similarly, if bleeding is accompanied by severe pain, increasing swelling, or signs of infection, you should not hesitate to contact your oral surgeon.
Your diligent adherence to post-operative care instructions is the single most important factor in ensuring a smooth recovery and preventing complications. This includes maintaining pressure on the surgical site with gauze, avoiding vigorous rinsing or spitting, refraining from smoking and alcohol, and sticking to a soft diet. Long-term, excellent oral hygiene and regular dental check-ups are paramount to the enduring health and success of your dental implant, helping you prevent future issues like peri-implantitis.
Remember, your dental care team is your best resource throughout this process. If you have any questions, concerns, or if something doesn’t feel right, always reach out to them. They have the expertise to assess your situation accurately and provide the best guidance for your specific needs, ensuring your journey to a restored smile is as comfortable and successful as possible.
Actionable Next Steps:
- Review Your Instructions: Re-read the post-operative care instructions provided by your dental surgeon.
- Monitor Your Symptoms: Keep a close eye on the amount and duration of any bleeding, as well as pain and swelling.
- Prepare Your Diet: Stock up on soft, cool foods and liquids to avoid irritating the surgical site.
- Have Contact Information Handy: Keep your dental surgeon’s contact information readily accessible in case you need to call them.
- Ask Questions: If anything is unclear or concerning, don’t hesitate to call your dental office.
References
[1] Al-Juboori, Z. A. (2020). Postoperative care and complications of dental implant surgery: A review. Journal of Baghdad College of Dentistry, 32(1), 170-176.
[2] Greenstein, G., Greenstein, B., & Kirsch, D. (2015). Peri-implantitis: a narrative review. Journal of Periodontology & Implant Science, 45(2), 58-69.
[3] Moy, P. K., & Wagner, J. A. (2007). Postoperative care following implant surgery. In Contemporary Implant Dentistry (pp. 531-546). Mosby Elsevier.

Leave a Reply
Share your thoughts or ask a question about dental implants. Your email address will not be published.