Imagine investing in a long-term solution for missing teeth, only to discover years later that your dental implant isn’t as stable as you hoped. It’s a distressing scenario, but understanding Late Dental Implant Failure – Symptoms & Prevention can empower you to protect your investment. While dental implants boast an impressive success rate, issues can sometimes arise long after the initial healing period. These late failures, occurring months or even years post-placement, are distinct from early failures and often stem from different underlying causes. Recognizing the warning signs and proactively preventing them is crucial for the longevity of your smile and overall oral health.
Key Takeaways
- Late dental implant failure occurs months or years after initial placement, typically due to bone density loss or poor maintenance.
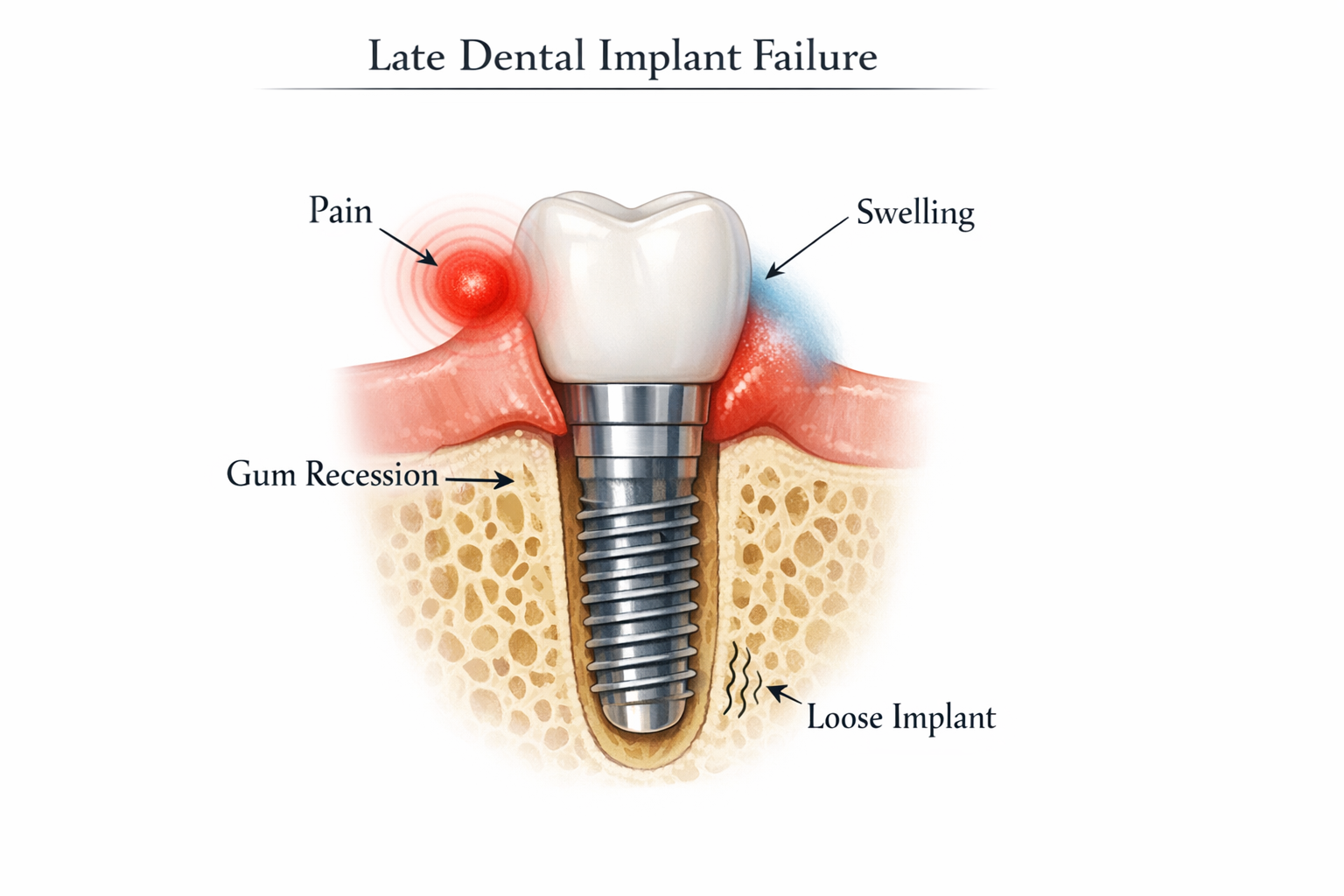
- Common symptoms include persistent pain, swelling, gum recession, implant mobility, and difficulty chewing.
- Major risk factors involve peri-implantitis (gum infection), systemic health conditions (like uncontrolled diabetes), smoking, and poor oral hygiene.
- Prevention is key, focusing on meticulous oral hygiene, regular dental check-ups, lifestyle modifications (quitting smoking), and prompt management of underlying health issues.
- Immediate action upon noticing symptoms is vital to save the implant and prevent further complications, requiring professional dental evaluation.
Understanding Late Dental Implant Failure: Symptoms to Watch For
Late dental implant failure refers to the loss of an implant’s stability and function well after the initial healing and osseointegration process (the fusion of the implant with the jawbone) has been completed. This can be particularly disheartening because patients have often enjoyed the benefits of their implants for an extended period. The primary culprits behind these late failures are typically loss of supporting bone density or inadequate ongoing care [1]. As an expert in oral health, I can attest that recognizing the signs early is paramount.
Here are the critical symptoms of late dental implant failure:
Persistent Pain or Discomfort
One of the most telling indicators of a problem is persistent pain or discomfort around the implant site. While some mild discomfort is normal immediately after surgery, chronic pain weeks or months later is a red flag. This pain can range from a dull ache to a sharp, throbbing sensation and may signal an infection, nerve impingement, or even the body’s rejection of the implant material. If you experience pain that doesn’t subside or worsens over time, it’s imperative to seek professional evaluation immediately.
Swelling, Redness, or Pus
Inflammation and infection are significant contributors to late implant failure. Symptoms such as swelling, redness, or the presence of pus near the implant are strong indicators of peri-implantitis. Peri-implantitis is a serious gum infection that mimics periodontal disease around natural teeth, but affects the tissues surrounding a dental implant [2]. This condition can erode the bone tissue supporting the implant, leading to its instability and eventual loss. If left untreated, peri-implantitis can rapidly progress and compromise the long-term success of your implant.
Implant Mobility or Looseness
A healthy dental implant should feel as stable and secure as a natural tooth. If you notice any mobility, wobbling, or a loose sensation when chewing or touching the implant, it suggests that osseointegration has failed or that the surrounding bone is deteriorating. This is a critical symptom requiring immediate attention. Unlike a loose natural tooth, an implant should not move at all. Any perceived movement, no matter how slight, indicates a significant issue with the implant’s integration with the jawbone.
Visible Gum Recession
Gum recession around the implant site, which exposes more of the metal post or the implant structure, is another concerning symptom. This can occur due to various factors, including aggressive brushing, thin gum tissue, or underlying infection. When gums recede, it not only impacts the aesthetics of your smile but also exposes the implant to bacteria, increasing the risk of infection and further bone loss. Healthy gums should tightly hug the implant, protecting it and the underlying bone.
Difficulty Chewing or Pressure Sensations
While dental implants are designed to restore full chewing function, difficulty or pain during chewing, biting, or experiencing unusual pressure sensations can signal mechanical issues or deeper bone loss around the implant. This could be due to a loose crown or abutment, but more seriously, it might indicate that the implant itself is no longer adequately supported by the jawbone. If your chewing experience changes dramatically or becomes uncomfortable, it’s a symptom not to be ignored.
Preventing Late Dental Implant Failure – Strategies for Long-Term Success
The good news is that many instances of late dental implant failure are preventable. By understanding the risk factors and committing to proactive measures, you can significantly increase the chances of your implants lasting a lifetime. Preventing Late Dental Implant Failure – Symptoms & Prevention involves a combination of meticulous oral hygiene, regular professional care, and healthy lifestyle choices.
Meticulous Oral Hygiene
This is arguably the most crucial aspect of preventing late implant failure. Just like natural teeth, dental implants require diligent cleaning to prevent plaque buildup and bacterial infections, particularly peri-implantitis.
- Brushing: Brush at least twice a day with a soft-bristled toothbrush. Consider an electric toothbrush designed for implant care. Pay close attention to the area where the implant meets the gum line.
- Flossing: Daily flossing is essential. Special implant-specific floss, interdental brushes, or water flossers can effectively clean around and between implants. For more details on the best products, you might want to read about the best dental implant aftercare products.
- Mouthwash: Use an antimicrobial mouthwash as recommended by your dentist to reduce bacterial load. Products like the best mouthwash for dental implants can be very beneficial.
Regular Dental Check-ups and Professional Cleanings
Even with excellent home care, professional oversight is indispensable. Regular dental check-ups, typically every six months, allow your dentist to:
- Monitor implant health: Your dentist will assess the surrounding gums and bone for any signs of inflammation or bone loss.
- Professional Cleanings: Special tools are used to clean implants without scratching their surface, removing stubborn plaque and calculus that home care might miss. This is different from cleaning natural teeth. For insights into costs, you can check out information on dental implant cleaning cost.
- Early Detection: Catching complications like peri-implantitis early can allow for intervention before irreversible damage occurs, potentially saving the implant.
Addressing Systemic Health Conditions
Certain uncontrolled systemic health conditions significantly impact the body’s ability to maintain implant stability and increase the risk of late failure.
- Diabetes: Uncontrolled diabetes impairs healing and increases susceptibility to infections. Managing blood sugar levels effectively is vital for implant longevity.
- Autoimmune Diseases: Conditions that affect the immune system can sometimes interfere with bone healing and increase inflammation around implants.
- Osteoporosis: While not a direct contraindication for implants, severe osteoporosis can affect bone density and the implant’s long-term stability. Discussion with your dentist and physician about managing this condition is important. You can learn more about how osteoporosis can affect teeth.
Lifestyle Modifications
Your daily habits play a significant role in the long-term success of your dental implants.
- Smoking Cessation: Smoking is one of the biggest risk factors for late implant failure. It impairs blood flow to the gums, slows healing, and compromises the bone’s ability to integrate with the implant. Quitting smoking dramatically improves implant prognosis. This is true for all dental procedures; even after a root canal, smoking is discouraged.
- Alcohol Consumption: Excessive alcohol intake can also hinder healing and increase infection risk. Moderation is key. For advice specific to implants, refer to guidelines on alcohol after dental implant surgery.
- Bruxism (Teeth Grinding): Chronic teeth grinding or clenching applies excessive force to implants, causing mechanical stress and accelerating bone deterioration. A nightguard can protect your implants and natural teeth from these forces.
- Avoid Hard Foods: Chewing on extremely hard objects (like ice, hard candies, or non-food items) can cause mechanical trauma to implants or their restorations. Be mindful of your diet, especially during the initial healing phases. Here’s a list of 50 soft foods after dental implant that can be helpful.
Prompt Treatment of Peri-Implantitis
If peri-implantitis is diagnosed, early and aggressive treatment is critical. This may involve:
- Professional Cleaning: Thorough cleaning to remove plaque and calculus from the implant surface.
- Antimicrobial Therapy: Local or systemic antibiotics to combat bacterial infection.
- Surgical Intervention: In more advanced cases, surgery may be necessary to debride the infected tissues, decontaminate the implant surface, and potentially graft bone to restore lost support.
Dental Implant Health Checklist 📝
Staying on top of your dental implant health is essential. Use this checklist as a quick guide to maintain your implants and prevent potential issues.
| Category | Action | Frequency | Importance |
|---|---|---|---|
| Oral Hygiene | Brush twice daily with a soft toothbrush | Daily | High |
| Floss daily (interdental brushes/water flosser) | Daily | High | |
| Use prescribed antimicrobial mouthwash | As directed | Medium | |
| Professional Care | Dental check-ups & professional cleanings | Every 6-12 months | High |
| X-rays to monitor bone levels | Annually or as needed | High | |
| Lifestyle | Avoid smoking and excessive alcohol | Continuous | High |
| Manage systemic diseases (e.g., diabetes) | Continuous | High | |
| Wear a nightguard if you grind teeth | Nightly (if applicable) | High | |
| Self-Monitoring | Check for pain, swelling, redness | Daily | High |
| Look for gum recession or exposed implant | Weekly | High | |
| Test for implant looseness (gently) | Monthly | High |
Note: This checklist is a general guide. Always follow your dental professional’s specific instructions.
What to Do If You Suspect Late Implant Failure

If you experience any of the symptoms of late dental implant failure, the most important step is to contact your dental professional immediately. Do not try to self-diagnose or wait for the symptoms to resolve on their own. Early intervention significantly improves the chances of saving the implant and preventing more complex, costly treatments down the line.
During your visit, your dentist will perform a thorough examination, which may include:
- Clinical Examination: Visually inspecting the implant, gums, and surrounding tissues for signs of inflammation, recession, or mobility.
- Probing: Gently measuring the depth of the gum pockets around the implant to assess for peri-implantitis.
- X-rays: Taking radiographs (X-rays) to evaluate the bone level around the implant and detect any signs of bone loss. This helps determine the extent of the problem and guides treatment decisions. You can learn more about CT scans and dental implants for diagnosis.
- Review of Medical History: Discussing any changes in your systemic health or medications that could impact implant health.
Based on these findings, your dentist will recommend an appropriate course of action. This could range from non-surgical treatments for early peri-implantitis to surgical interventions or, in severe cases, removal of the failing implant. Our team is committed to providing comprehensive care, and you can learn more about our philosophy on our About Us page.
The Importance of a Proactive Approach
Maintaining dental implants is a long-term commitment. Think of it like maintaining your natural teeth, but with a few special considerations. A proactive approach not only helps prevent Late Dental Implant Failure – Symptoms & Prevention but also ensures the overall health of your mouth. Choosing the right specialists for your initial implant procedure is also crucial, as their expertise can minimize risks. If you’re considering implants, it’s wise to consult with experienced professionals, such as those at dentalimplantsdallastx.com.
Regular communication with your dental team is vital. If you have any concerns or notice even subtle changes around your implant, don’t hesitate to reach out. Your dental team is your best resource for guidance and support in maintaining a healthy, functional smile for years to come. Remember, proper care can mean the difference between lasting success and preventable failure.
Conclusion
Dental implants offer a remarkable solution for tooth replacement, providing excellent stability, function, and aesthetics. However, their long-term success hinges on understanding and actively addressing potential challenges like late dental implant failure. By being vigilant about the symptoms—such as persistent pain, swelling, gum recession, or mobility—and by diligently following prevention strategies, you can significantly safeguard your investment. Meticulous oral hygiene, regular professional check-ups, managing systemic health conditions, and adopting a healthy lifestyle are not just recommendations; they are essential pillars for ensuring the longevity of your dental implants. If you suspect any issues, immediate consultation with your dental professional is the most critical step to prevent further complications and preserve your oral health.
Actionable Next Steps:
- Self-Assess: Regularly check your dental implants for any of the symptoms discussed (pain, swelling, gum recession, looseness).
- Schedule a Check-up: If it’s been more than six months, schedule a professional cleaning and check-up with your dentist, especially if you have implants.
- Optimize Oral Hygiene: Ensure you are brushing twice daily and flossing around your implants with appropriate tools.
- Review Lifestyle: Reflect on your smoking habits, alcohol consumption, and diet, making changes to support optimal implant health. If you grind your teeth, discuss a nightguard with your dentist.
- Manage Health Conditions: Work with your doctor to ensure any systemic health conditions (like diabetes) are well-managed.
References
[1] Alsaeed, T. A., & Al-Ahmari, R. (2020). Risk factors for late dental implant failure: A systematic review. Journal of Oral Implantology, 46(4), 312-321.
[2] Renvert, S., & Polyzois, I. (2018). Clinical advances in the diagnosis and management of peri-implant diseases. Periodontology 2000, 76(1), 163-171.
Dental Implant Late Failure Risk Assessment
Answer these questions to get an estimated risk level for late dental implant failure and personalized prevention tips. This tool is for informational purposes only and does not replace professional dental advice.
Your Dental Implant Risk Assessment
Risk Level: Moderate
- Continue your excellent oral hygiene.

Leave a Reply
Share your thoughts or ask a question about dental implants. Your email address will not be published.