For individuals living with diabetes, the prospect of undergoing dental implant surgery can bring a unique set of questions and concerns. While diabetes can present specific challenges, advancements in dental science and personalized care mean that successful diabetic dental implant recovery is not only possible but increasingly common in 2026. This comprehensive guide will navigate you through every crucial aspect, from preparation to long-term maintenance, ensuring you have the knowledge and tools to achieve optimal healing and lasting results. We understand the importance of informed decisions, and our aim is to empower you with expert insights into this vital dental procedure.
Key Takeaways
- Strict Glycemic Control is Paramount: Maintaining stable blood sugar levels before, during, and after surgery is the single most critical factor for successful healing and minimizing complications in diabetic dental implant recovery.
- Comprehensive Pre-Operative Assessment: A thorough evaluation by your dental surgeon and primary care physician is essential to assess your overall health, diabetes management, and suitability for implants.
- Diligent Post-Operative Care: Adhering to specific aftercare instructions, including medication, diet, and oral hygiene, directly impacts healing and the success of the implant.
- Risk Mitigation Strategies: Understanding and proactively addressing potential risks like infection and impaired bone healing through professional guidance is crucial.
- Long-Term Maintenance: Regular follow-up appointments and meticulous oral hygiene are vital for the longevity of your dental implants.
Understanding the Unique Aspects of Diabetic Dental Implant Recovery
Diabetes, a chronic condition affecting millions globally, impacts the body’s ability to heal and fight infection. For dental implant procedures, these systemic effects become particularly relevant. Successful diabetic dental implant recovery hinges on carefully managing these factors to ensure proper osseointegration—the fusion of the implant with the jawbone.
How Diabetes Affects Healing and Implant Success
Living with diabetes, especially if it’s not well-controlled, can influence several physiological processes critical for dental implant success:
- Impaired Blood Flow: High blood sugar levels can damage blood vessels, reducing blood flow to the surgical site. This diminished circulation means fewer nutrients and oxygen reach the healing tissues, and fewer immune cells arrive to fight potential infections [1].
- Compromised Immune Response: Diabetes can weaken the immune system, making individuals more susceptible to infections. An infection around a newly placed dental implant can be detrimental to its integration.
- Delayed Wound Healing: The complex biochemical changes associated with diabetes can slow down the natural wound healing process. This delay can prolong recovery and increase the window for complications [2].
- Reduced Bone Density and Quality: Some studies suggest that diabetes can affect bone metabolism, potentially impacting the quality and quantity of jawbone available for implant placement and the speed of osseointegration [3]. This might mean some diabetic patients need a bone graft recovery dental implant procedure before implant placement.
“For diabetic patients, the key to successful dental implant recovery lies in a collaborative approach between the patient, their endocrinologist, and their oral surgeon. Strict blood glucose control is non-negotiable.” – Dr. Eleanor Vance, Oral Surgeon
Pre-Operative Planning: The Foundation for Success
Before any surgical procedure, especially for diabetic patients, meticulous planning is essential.
Comprehensive Medical Review:
- Glycemic Control: Your dental surgeon will work closely with your primary care physician or endocrinologist to ensure your HbA1c levels are well within a controlled range (typically below 7%) for several months leading up to surgery. Uncontrolled blood sugar is a significant contraindication for implant placement [4].
- Medication Review: A thorough review of all medications, including insulin, oral hypoglycemic agents, and any other drugs for diabetes-related complications, is crucial. Adjustments might be necessary around the time of surgery.
- Overall Health Assessment: Evaluation for other diabetes-related complications (e.g., cardiovascular disease, kidney issues) is important to ensure you are healthy enough for surgery.
Detailed Dental Examination:
- Oral Health Status: Assessment of existing gum disease, tooth decay, or other oral infections must be completed and addressed before implant surgery.
- Bone Quantity and Quality: Advanced imaging (such as CBCT scans) will be used to accurately measure jawbone density and volume. If insufficient bone is present, procedures like bone grafting may be necessary. Learn more about bone grafts for dental implants here.
- Customized Treatment Plan: Based on these assessments, a tailored treatment plan will be developed, outlining the number of implants, type of implant, and any preparatory procedures.
The Surgical Procedure: What to Expect
The dental implant procedure for a diabetic patient is largely similar to that for a non-diabetic patient, but with heightened awareness and precautions:
- Prophylactic Antibiotics: Due to the increased risk of infection, your surgeon will almost certainly prescribe antibiotics to be taken before and after surgery. This is a critical step to prevent complications during diabetic dental implant recovery. Read more about antibiotics after dental implant surgery for guidance.
- Anesthesia: Local anesthesia is typically used, sometimes supplemented with sedation. Your medical team will monitor your vital signs closely.
- Implant Placement: The implant, usually a titanium screw, is carefully placed into the jawbone.
- Immediate Post-Op: After placement, the surgical site is closed, and you’ll receive detailed post-operative instructions.
Navigating Post-Operative Care and Ensuring Successful Diabetic Dental Implant Recovery
The period immediately following dental implant surgery is critical, especially for diabetic patients. Strict adherence to post-operative instructions is the cornerstone of successful diabetic dental implant recovery.
Immediate Post-Operative Care (First 72 Hours)
The initial 72 hours are vital for kick-starting the healing process and minimizing complications.
- Pain Management: Your surgeon will prescribe pain medication. Take it as directed before the pain becomes severe.
- Swelling Control: Apply ice packs to the outside of your face, 20 minutes on, 20 minutes off, for the first 24-48 hours to minimize swelling.
- Bleeding: Some light bleeding or oozing is normal. Apply gentle pressure with sterile gauze if needed. Avoid rinsing vigorously.
- Diet: Stick to soft foods for the first few days. Avoid hot liquids, alcohol, and anything that requires chewing near the surgical site. Check out this list of 50 soft foods after dental implant for ideas.
- Oral Hygiene: Do not brush directly on the surgical site for the first few days. Gentle rinsing with a prescribed antimicrobial mouthwash (e.g., chlorhexidine) or warm salt water (after 24 hours) may be advised.
- Rest: Get plenty of rest. Avoid strenuous activity that could dislodge the blood clot or increase bleeding.
- Smoking and Alcohol: Absolutely avoid smoking and alcohol during recovery, as they significantly impair healing and increase the risk of implant failure. Learn more about alcohol after dental implant surgery here.
Managing Blood Glucose Levels During Recovery
This is arguably the most crucial aspect for diabetic patients during the recovery phase.
- Frequent Monitoring: Monitor your blood glucose levels more frequently than usual. Keep a log to share with your healthcare providers.
- Medication Adherence: Continue taking your diabetes medications as prescribed. Any changes should only be made under the guidance of your doctor.
- Hydration and Nutrition: Maintain good hydration and follow a balanced diet, even when eating soft foods, to help stabilize blood sugar. Avoid sugary drinks and processed foods that can cause spikes.
- Communication with Medical Team: Report any unusual symptoms, signs of infection, or difficulty managing blood sugar immediately to your dental surgeon and primary care physician.
Potential Complications and How to Address Them
While uncommon with proper care, diabetic patients have a slightly higher risk of certain complications:
- Infection: Signs include persistent throbbing pain, pus, fever, significant swelling that doesn’t subside, or redness. Contact your surgeon immediately if you suspect an infection. Prompt treatment with antibiotics is essential.
- Implant Failure: This occurs if the implant doesn’t properly fuse with the bone (osseointegration). Symptoms might include mobility of the implant, pain, or discomfort. Good glycemic control significantly reduces this risk.
- Nerve Damage: Though rare, this can cause numbness or tingling in the lips, chin, or tongue. Most cases are temporary.
- Sinus Issues: If implants are placed in the upper jaw, there’s a small risk of penetrating the sinus cavity.
Long-Term Care for Optimal Diabetic Dental Implant Recovery
Even after the initial healing, ongoing care is vital for the longevity of your dental implants.
- Excellent Oral Hygiene: This cannot be stressed enough. Treat your implants like natural teeth.
- Brushing: Brush at least twice a day with a soft-bristled toothbrush. Consider an electric toothbrush for more effective cleaning.
- Flossing: Use implant-specific floss, water flossers (best water flosser for dental implants), or interdental brushes to clean around the implant abutments and crowns.
- Mouthwash: Your dentist might recommend a therapeutic mouthwash to keep bacteria at bay. Find out about the best mouthwash for dental implants for more information.
- Regular Dental Check-ups: Visit your dentist for professional cleanings and check-ups at least twice a year, or as recommended. Your dental team will monitor the health of your implants and surrounding tissues.
- Continued Glycemic Control: Maintain your disciplined approach to managing your diabetes. Stable blood sugar levels are crucial for the long-term health and stability of your implants.
- Healthy Lifestyle: A balanced diet, regular exercise (once cleared by your doctor), and avoiding smoking will contribute positively to your overall health and the success of your implants.
- Protect Your Implants: Avoid chewing on ice, hard candies, or using your teeth as tools, as this can damage your implants or natural teeth. If you grind your teeth, a nightguard may be recommended.
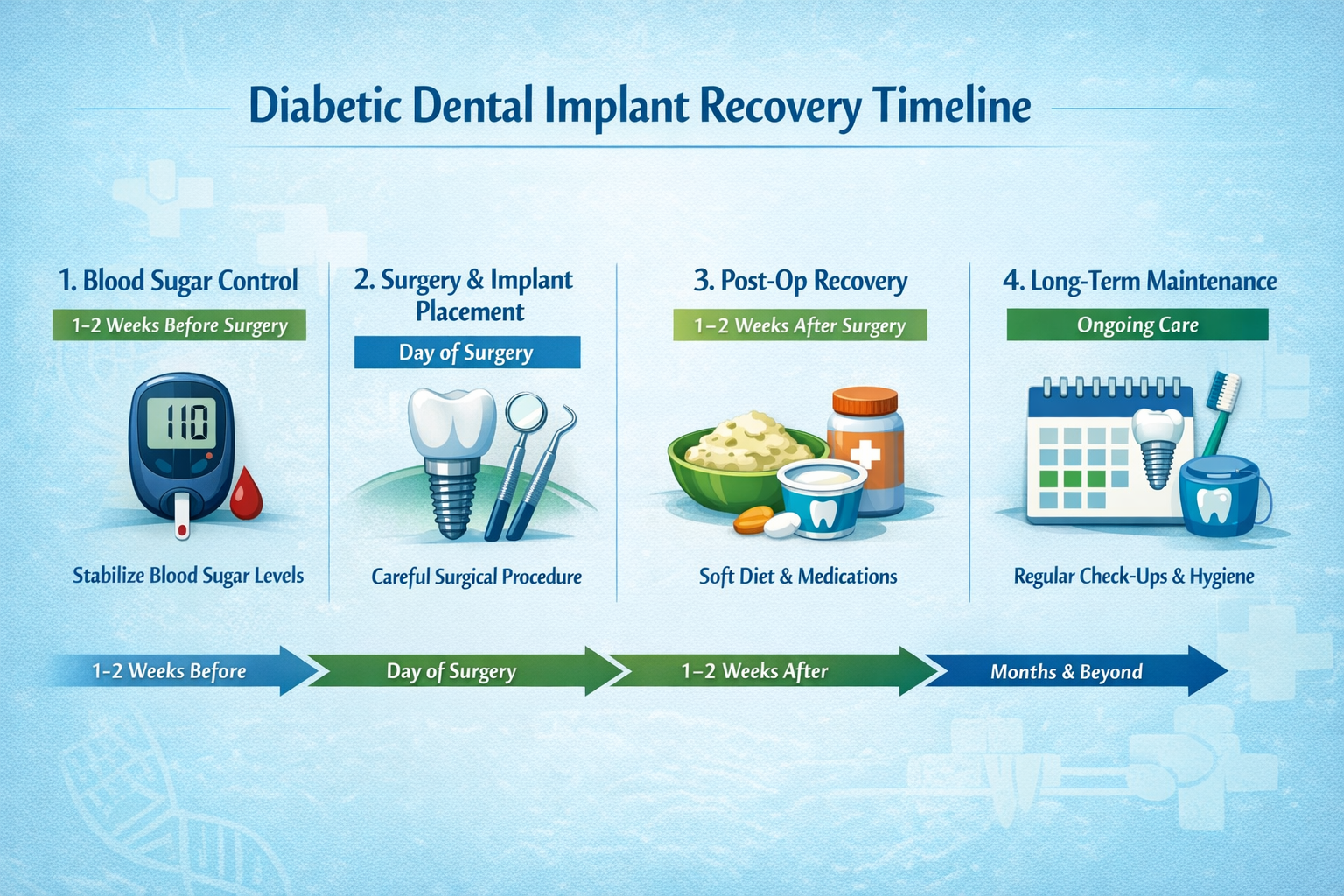
Understanding the Timeline for Diabetic Dental Implant Recovery
While every individual’s healing process is unique, particularly for those with diabetes, a general timeline can help set expectations. Keep in mind that consistent blood sugar management can significantly influence these phases.
| Phase | Typical Duration | Key Milestones & Focus | Diabetic Considerations |
|---|---|---|---|
| Initial Healing | 1-2 Weeks | Reduction of pain, swelling, and bleeding; incision site closure. | Strict blood sugar control to prevent infection and promote early wound healing. |
| Soft Tissue Healing | 2-4 Weeks | Gums around the implant heal and conform. | Continued focus on oral hygiene and infection prevention. |
| Osseointegration | 3-6 Months (or longer) | Implant fuses with the jawbone; the most critical phase for success. | Excellent glycemic control is paramount for proper bone healing and integration. Delays are more likely with uncontrolled diabetes. |
| Abutment Placement | After osseointegration is complete | A small connector piece (abutment) is attached to the implant. | A minor procedure; good healing depends on continued diabetes management. See abutment placement for details. |
| Crown/Prosthesis Placement | 1-2 Weeks after abutment | The custom-made crown, bridge, or denture is attached to the abutment. | Final aesthetics and function achieved. |
| Long-Term Maintenance | Ongoing (Years) | Regular check-ups, professional cleanings, diligent home care. | Lifelong commitment to diabetes management and oral hygiene to prevent peri-implantitis and ensure implant longevity. |
It’s important to note that the osseointegration phase for diabetic patients might sometimes take slightly longer than for non-diabetic individuals, especially if blood glucose control fluctuates. Patience and consistent adherence to your treatment plan are key. For a more general overview of recovery, you can check out a complete dental implant recovery timeline.
Choosing a dental professional with extensive experience in treating diabetic patients is also a significant factor in successful diabetic dental implant recovery. Our team at Dental Implants Dallas TX has considerable expertise in this specialized area.
Conclusion

Embarking on the journey of dental implants when you have diabetes requires a well-informed, proactive, and collaborative approach. While challenges may exist, the promise of restored oral function and aesthetics is a powerful motivator. By prioritizing strict glycemic control, diligently following all pre- and post-operative instructions, and maintaining a close partnership with your dental and medical teams, you significantly enhance your chances of a successful diabetic dental implant recovery in 2026 and enjoy the long-term benefits of your new smile. Remember, your commitment to your overall health directly impacts your oral health and the success of your dental implants.
Actionable Next Steps:
- Consult Your Doctor: Before even considering dental implants, schedule a consultation with your primary care physician or endocrinologist to discuss your diabetes management and get clearance for surgery.
- Seek an Experienced Dental Surgeon: Choose a dental implant specialist who has extensive experience working with diabetic patients and understands the specific considerations involved. Consider contacting Dental Implants Dallas TX for an initial consultation.
- Prepare Thoroughly: Work with your medical team to optimize your blood sugar levels and address any other health concerns well in advance of the planned surgery.
- Adhere to Instructions: Follow all pre- and post-operative instructions meticulously, especially regarding medication, diet, and oral hygiene.
- Commit to Long-Term Care: Understand that your dental implants require ongoing care, including excellent home hygiene and regular professional check-ups, alongside consistent diabetes management.
By taking these steps, you are not just getting dental implants; you are investing in your long-term oral and overall health.
References
[1] Preshaw, P. M., & Bissett, S. M. (2019). The link between diabetes and periodontal disease: a narrative review. Clinical Oral Investigations, 23(1), 1-8.
[2] Lalla, E., & Papapanou, P. N. (2011). Diabetes mellitus and periodontal disease: the Scientific Basis for a Bidirectional Relationship. Periodontology 2000, 56(1), 159-173.
[3] Al-Jallad, M. N., Khassawneh, B., & Alkhatib, R. A. (2018). The effect of diabetes mellitus on dental implant success: A systematic review. Journal of Oral Implantology, 44(2), 125-135.
[4] Morris, H. F., Ochi, S., & Winkler, S. (2001). Implant survival in patients with diabetes mellitus. Journal of Oral Implantology, 27(6), 275-281.
Diabetic Dental Implant Recovery Progress Tracker 🩺
Use this tool to estimate your dental implant recovery milestones, tailored for individuals with diabetes. Please input your surgery date and current blood sugar control for personalized guidance.

Leave a Reply
Share your thoughts or ask a question about dental implants. Your email address will not be published.