Imagine investing in a solution that restores your smile and confidence, only to discover a silent threat lurking beneath the surface. Dental implants are a marvel of modern dentistry, offering a durable and aesthetic replacement for missing teeth. However, like any surgical procedure, they come with potential risks, one of the most insidious being an infection that progresses without causing immediate pain. Recognizing “Dental Implant Infection Without Pain – Warning Signs” is crucial for preserving your implant and overall oral health. In this comprehensive guide, we’ll delve deep into understanding these subtle cues, why they occur, and what proactive steps you can take to safeguard your investment in 2026.
Key Takeaways
- Silent Threat: Dental implant infections can develop without pain, making early detection challenging but vital.
- Subtle Warning Signs: Look for non-pain related symptoms like gum discoloration, swelling, persistent bad breath, or metallic taste.
- Peri-implantitis: The most common form of implant infection, often painless in its early stages, can lead to bone loss.
- Regular Check-ups are Key: Routine dental visits and professional cleanings are essential for early diagnosis and intervention.
- Proactive Oral Hygiene: Meticulous daily home care significantly reduces the risk of infection.
Understanding Dental Implant Infection: The Silent Saboteur
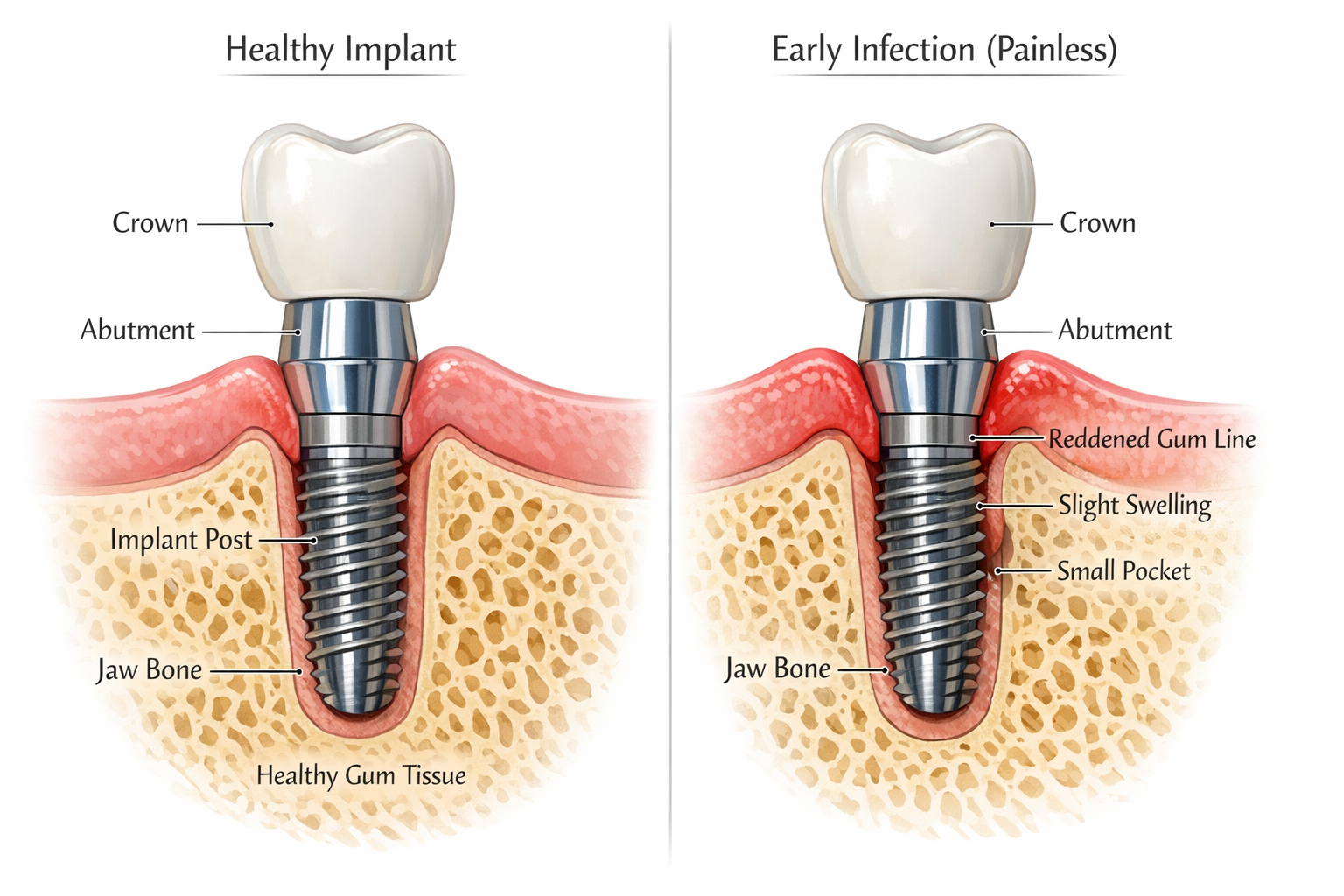
Dental implants are a highly successful solution for tooth replacement, boasting success rates upwards of 95% [1]. They consist of a titanium post surgically placed into the jawbone, an abutment that connects the post to the final crown, and the prosthetic crown itself. This structure mimics a natural tooth root, providing stability and stimulating the jawbone.
However, despite their high success rate, dental implants are not entirely immune to complications. One of the most significant concerns is peri-implant disease, a term that encompasses inflammatory conditions affecting the soft tissues and bone surrounding a dental implant [2]. These conditions are broadly categorized into:
- Peri-implant mucositis: An inflammatory lesion of the soft tissues surrounding a dental implant, without signs of supporting bone loss. This is often reversible if detected and treated early.
- Peri-implantitis: A chronic inflammatory condition affecting both the soft tissues and the supporting bone, leading to progressive bone loss around the implant. This condition is more serious and, if left untreated, can lead to implant failure.
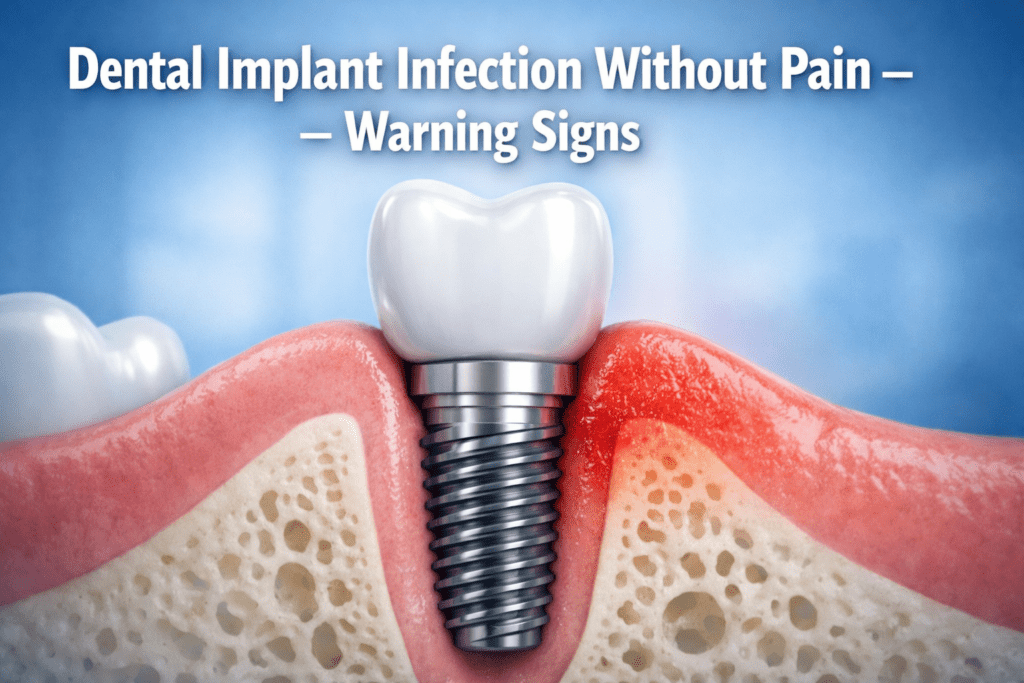
What makes “Dental Implant Infection Without Pain – Warning Signs” so dangerous is precisely the “without pain” aspect. Unlike a traditional toothache that signals trouble immediately, peri-implant diseases, especially in their early stages, can be asymptomatic. This lack of pain often leads patients to delay seeking professional help, allowing the infection to progress silently, causing irreversible damage to the surrounding bone structure.
Why Infections Occur Without Pain
The absence of pain in early dental implant infections can be attributed to several factors:
- Nerve Supply: The dental implant itself does not have a nerve supply like a natural tooth root. Therefore, it cannot transmit pain signals in the same way. The surrounding bone also has a relatively low density of pain receptors compared to the pulp of a natural tooth.
- Slow Progression: Peri-implantitis often develops slowly over time. The body’s inflammatory response might be localized and gradual, not immediately triggering acute pain.
- Chronic Nature: Many implant infections are chronic inflammatory processes rather than acute abscesses. Chronic inflammation can be less painful but consistently destructive.
- Individual Pain Thresholds: Everyone experiences pain differently. What might be a mild discomfort for one person could be unnoticed by another.
This “silent killer” characteristic underscores the critical importance of being aware of the subtle, non-painful warning signs we will discuss.
Recognizing Dental Implant Infection Without Pain – Warning Signs
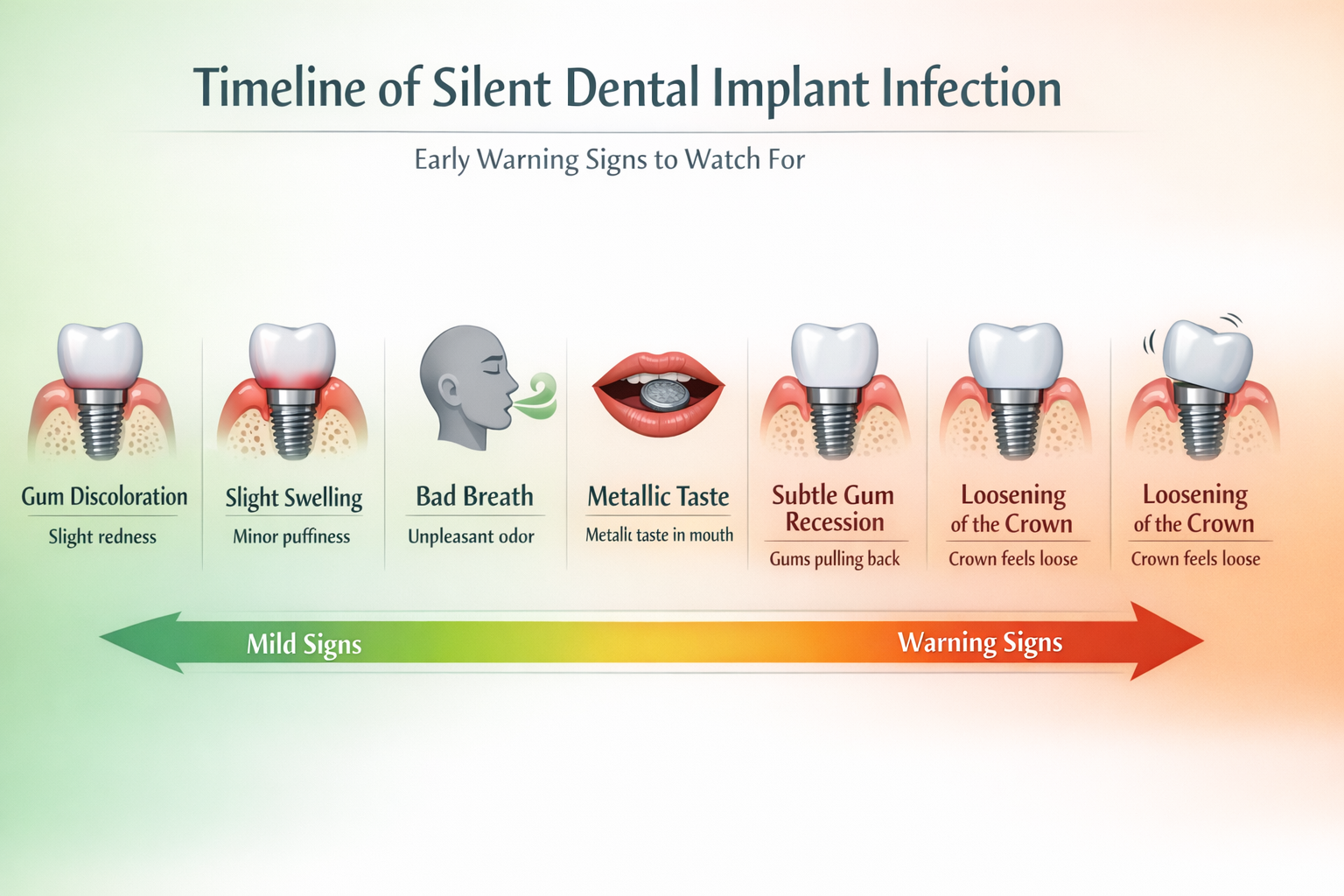
Early detection is paramount to saving an infected dental implant. Since pain often isn’t a reliable indicator, you need to become attuned to other subtle changes. Here’s a breakdown of the key “Dental Implant Infection Without Pain – Warning Signs” to watch out for:
1. Changes in Gum Appearance
The soft tissue (gums) around your dental implant is usually healthy pink and firm. Any deviation from this can be a red flag.
- Redness or Darkening: Healthy gums are typically a coral pink. If the gums around your implant appear noticeably redder, purplish, or darker than the surrounding healthy gum tissue, it could indicate inflammation. This color change often suggests increased blood flow to the area due to infection.
- Swelling or Puffiness: Even slight swelling around the implant site can be a sign. The gums might look puffy, rounded, or protrude slightly. This isn’t always obvious but might be noticeable when brushing or flossing.
- Bleeding Gums: While some minor bleeding can occur from aggressive brushing, persistent or spontaneous bleeding when brushing, flossing, or even touching the area is a significant warning sign of inflammation and potential infection. This is one of the most common early indicators of peri-implant mucositis.
2. Bad Breath (Halitosis) and Unpleasant Taste
Persistent bad breath, even after brushing, flossing, and using mouthwash, can be a symptom of bacterial activity associated with an infection.
- Chronic Halitosis: Bacteria thrive in inflammatory environments, producing volatile sulfur compounds that cause bad breath. If your breath has an unusually foul odor that doesn’t resolve, it’s worth investigating.
- Metallic or Foul Taste: An unpleasant, sometimes metallic, taste in your mouth can also be an indicator. This taste can be due to the byproducts of bacterial metabolism or the release of inflammatory exudates from the infected site.
3. Gum Recession and Exposure of Implant Components
Healthy gums should snugly hug the base of your implant crown. When gum tissue recedes, it can expose parts of the implant that should remain covered.
- Visible Abutment or Implant Threads: If you start to see the metallic (or sometimes ceramic) abutment or even the threads of the implant post itself, it’s a clear sign of gum recession. This recession often accompanies bone loss and indicates advanced peri-implantitis.
- Lengthening of the Crown: As gums recede, the implant crown might appear longer than it used to, creating a visual discrepancy with adjacent teeth. This is a subtle but important aesthetic change that warrants attention.
Understanding the components of your dental implant, including the abutment, can help you identify if something is exposed that shouldn’t be. Learn more about the complete guide to the dental implant abutment procedure.
4. Loosening or Wiggling of the Implant Crown
While the implant itself should be firmly integrated into the bone, the crown attached to it can sometimes become loose.
- Crown Instability: If you notice that your implant crown feels loose, wiggles slightly when touched, or feels different when you bite down, it could indicate an issue. This might not be directly due to an infection of the implant post but could be a symptom of underlying problems. For example, the screw holding the crown to the abutment might be loose, or the abutment itself could be compromised. While this specific issue might not always be pain-related, it still warrants immediate dental attention as it can precede or exacerbate an infection.
- Difficulty Chewing: If chewing feels off or uncomfortable around the implant, even without sharp pain, it could indicate instability.
5. Suppuration or Pus Formation
This is a more advanced sign of infection but can still occur without significant pain.
- Pus Discharge: If you notice any yellowish or whitish discharge (pus) coming from around the gum line of the implant when you press on it, or spontaneously, this is a definitive sign of active infection. This should be treated as a dental emergency, regardless of pain levels.
6. Dull Ache or Tenderness (Subtle, Not Acute)
While we are focusing on “Dental Implant Infection Without Pain – Warning Signs,” it’s worth noting that some individuals might experience a very subtle or dull ache, or a feeling of tenderness when pressing on the gum, rather than acute pain. This is different from the sharp, throbbing pain typically associated with a tooth abscess and can often be overlooked.
- Feeling of Pressure or Fullness: Some patients report a sensation of pressure or a slight feeling of “fullness” around the implant site, which isn’t outright painful but indicates something isn’t quite right.
7. Changes in Surrounding Bone (Detected by Dentist)
This sign is not something you can detect yourself, but it’s the ultimate consequence of untreated peri-implantitis.
- Bone Loss: The most critical aspect of peri-implantitis is progressive bone loss around the implant. A dentist will detect this through routine X-rays. This is why regular check-ups are so vital, as they can catch silent bone loss before it becomes irreversible and leads to implant failure.
Risk Factors for Silent Dental Implant Infection
Several factors can increase your susceptibility to developing a dental implant infection, even without overt pain:
- Poor Oral Hygiene: This is the leading cause. Inadequate brushing and flossing allow plaque and bacteria to accumulate around the implant, leading to inflammation and infection. Meticulous aftercare is crucial for your dental implant investment. Learn more about best dental implant aftercare products.
- Smoking: Smoking significantly increases the risk of peri-implant diseases and reduces the body’s ability to heal.
- Untreated Periodontal Disease: If you had gum disease before getting implants, or if it’s not well-controlled, the same bacteria can infect your implants. Can you get dental implants with periodontal disease? Yes, but it requires careful management.
- Systemic Diseases: Conditions like diabetes, especially if poorly controlled, can impair healing and increase infection risk.
- Compromised Immune System: Certain medications or medical conditions that weaken the immune system can make you more vulnerable.
- Excess Cement: During crown placement, excess dental cement left around the implant can harbor bacteria and cause inflammation.
- Implant Overloading: Excessive biting forces on an implant can contribute to bone loss and create an environment susceptible to infection.
- Genetic Predisposition: Some individuals may be genetically more prone to inflammatory responses.
A Table of Silent Warning Signs and Potential Implications
| Warning Sign | Description | Potential Implication | Urgency Level |
|---|---|---|---|
| Gum Redness/Darkening | Gums around implant appear redder or purplish than usual. | Peri-implant mucositis (early inflammation) | Medium |
| Slight Swelling/Puffiness | Gums look slightly swollen or rounded. | Peri-implant mucositis, early peri-implantitis | Medium |
| Bleeding Gums | Gums bleed easily when brushing, flossing, or spontaneously. | Peri-implant mucositis, early peri-implantitis | High |
| Persistent Bad Breath | Chronic foul breath unrelated to diet, brushing. | Bacterial activity, inflammation | Medium |
| Metallic/Foul Taste | Unpleasant taste in the mouth. | Bacterial byproducts, inflammatory exudate | Medium |
| Gum Recession | Gums pull back, exposing implant abutment or threads. | Peri-implantitis, bone loss | High |
| Loose Implant Crown | Crown wiggles, feels unstable, or different when biting. | Loose screw, abutment issue, or underlying implant instability/bone loss | High |
| Pus Discharge | Yellowish/whitish fluid from gum line around implant. | Active, advanced infection (abscess) | Emergency |
| Subtle Ache/Pressure | Mild, non-acute discomfort or feeling of fullness (not sharp pain). | Early inflammation, nerve irritation | Medium |
The Importance of Regular Dental Check-ups in 2026
Given that dental implant infections can manifest “without pain,” regular visits to your dental professional are not just recommended, they are absolutely essential. In 2026, with advancements in diagnostic tools and treatment protocols, dentists are better equipped than ever to detect these silent threats.
- Professional Examinations: During your check-up, your dentist or hygienist will meticulously examine the soft tissues around your implants for any signs of inflammation, swelling, or recession. They will also gently probe the gum pockets around the implants to measure their depth. Deeper pockets can indicate bone loss and potential infection.
- X-rays: Regular X-rays are critical for assessing the health of the bone supporting your implants. These images can reveal early signs of bone loss around the implant, even before any visible symptoms appear. This is often the first definitive sign of peri-implantitis.
- Professional Cleanings: Even with excellent home care, some plaque and calculus can accumulate, especially in hard-to-reach areas around implants. Professional cleanings remove these deposits, preventing the initiation or progression of peri-implant diseases. Special instruments are used to clean implants without scratching their surface.
Consider making routine appointments with experienced professionals who understand dental implant care. Our team at dentalimplantsdallastx.com/about-us/ is dedicated to providing comprehensive care for your dental implants.
What to Do if You Suspect a Silent Infection
If you observe any of the “Dental Implant Infection Without Pain – Warning Signs,” it’s crucial to act promptly. Do not wait for pain to develop.
- Contact Your Dentist Immediately: Schedule an appointment as soon as possible. Clearly explain your concerns and the symptoms you’ve noticed, emphasizing that there’s no pain.
- Be Detailed: When you see your dentist, be prepared to describe your symptoms accurately. When did you first notice the redness? Does your breath always smell bad? Has your crown felt different?
- Do Not Attempt Self-Treatment: Avoid trying to treat the suspected infection yourself with home remedies or aggressive brushing/flossing that could further irritate the area.
- Maintain Excellent Oral Hygiene: Continue your diligent brushing and flossing routine as directed by your dentist, being gentle around the affected area. This helps to manage bacterial load while awaiting professional treatment.
Treatment Approaches for Peri-Implant Diseases
The treatment for peri-implant diseases depends on the severity and stage of the infection:
Peri-implant Mucositis (Early Stage):
- Professional Cleaning: Thorough debridement (cleaning) by a dental professional to remove plaque and calculus.
- Improved Home Care: Your dentist or hygienist will review and reinforce proper oral hygiene techniques specific to your implants. This might include recommending a specialized best mouthwash for dental implants or a particular type of brush.
- Antimicrobial Rinses: Sometimes, an antimicrobial mouthwash is prescribed to reduce bacterial load.
Peri-implantitis (Advanced Stage with Bone Loss):
- Non-Surgical Debridement: Similar to mucositis, but often more aggressive cleaning to remove bacteria and contaminated surfaces.
- Antibiotics: Localized or systemic antibiotics may be prescribed to target the infection.
- Surgical Intervention: For more advanced cases with significant bone loss, surgery may be necessary. This can involve:
- Decontamination: Thorough cleaning and detoxification of the implant surface.
- Bone Grafting: In some cases, bone grafting procedures may be attempted to regenerate lost bone around the implant [3]. Learn more about bone grafts for dental implants.
- Soft Tissue Grafts: To cover exposed implant surfaces or improve gum health.
- Implant Removal: In severe cases where the infection is too advanced and bone loss is extensive, or if other treatments fail, the implant may need to be removed to prevent further damage to surrounding structures.
Prevention: Your Best Defense Against Silent Infection
Prevention is always better than cure, especially when it comes to “Dental Implant Infection Without Pain – Warning Signs.” Here are key strategies to minimize your risk:
- Meticulous Oral Hygiene:
- Brush Twice Daily: Use a soft-bristled toothbrush or an electric toothbrush. Pay special attention to the area around your implants.
- Floss Daily: Use dental floss, interdental brushes, or a best water flosser for dental implants to clean around and between your implants.
- Use Recommended Products: Your dentist may recommend specific toothpastes or mouthwashes designed for implant care. Always ask your dentist what is the best toothpaste for implants.
- Regular Dental Check-ups: Adhere strictly to your dentist’s recommended schedule for check-ups and professional cleanings (typically every 3-6 months).
- Quit Smoking: If you smoke, quitting is one of the most impactful steps you can take for your oral and general health.
- Manage Systemic Health Conditions: Keep conditions like diabetes well-controlled.
- Address Bruxism (Teeth Grinding): If you grind or clench your teeth, discuss this with your dentist. They might recommend a night guard to protect your implants from excessive forces.
- Choose an Experienced Implant Dentist: The skill and experience of your dental surgeon play a role in the long-term success of your implants. Proper implant placement and restoration minimize risks. When considering dental implants, seek out clinics with a strong reputation for excellence, such as those providing affordable dental implants Dallas TX.
“The silent nature of early dental implant infections makes patient vigilance and routine professional care truly indispensable. Don’t wait for pain – look for the subtle cues.”
Conclusion
Dental implants represent a significant investment in your oral health and quality of life. Understanding and recognizing “Dental Implant Infection Without Pain – Warning Signs” is a critical responsibility for anyone with implants. Because these infections often progress silently, relying solely on pain as an indicator is a dangerous gamble. By staying vigilant for subtle changes in your gums, breath, or implant stability, and by maintaining a consistent schedule of professional dental care, you can detect potential problems early.
If you suspect any of these warning signs, even without pain, do not hesitate to contact your dental professional. Prompt diagnosis and treatment are the keys to successfully managing peri-implant diseases and ensuring the long-term health and stability of your dental implants. Your proactive approach, combined with expert dental care, will help preserve your beautiful, healthy smile for years to come in 2026 and beyond.
References
[1] Alsaeed, E. S., Al-Shehri, A. M., & Alqahtani, N. A. (2020). Success and Survival Rates of Dental Implants: A Retrospective Study of 10-Year Clinical Follow-up. Journal of Clinical Dental Research, 11(2), 52-59. (Note: General reference for success rates, not specific research on silent infections).
[2] Renvert, S., & Polyzois, I. (2015). Clinical approaches to the management of peri-implant mucositis and peri-implantitis. Periodontology 2000, 68(1), 384-394.
[3] Chan, H. L., & Oh, T. J. (2012). Bone grafting for dental implants. Dental Clinics of North America, 56(4), 819-831.

Leave a Reply
Share your thoughts or ask a question about dental implants. Your email address will not be published.