Embarking on the journey to restore a confident smile often involves dental implant placement. A critical phase in this process, often less discussed but equally vital, is the intricate period of dental implant tissue punch healing. This article delves deep into understanding the tissue punch procedure, the subsequent healing phases, and how to ensure the best possible outcomes for your oral health in 2026 and beyond. Whether you are considering dental implants, have recently undergone the procedure, or simply seek to understand the science behind this modern dental marvel, this comprehensive guide will provide clarity and valuable insights. The success of a dental implant relies heavily on the proper integration with both bone and surrounding soft tissues, making the healing process post-tissue punch a cornerstone of long-term success.
Key Takeaways
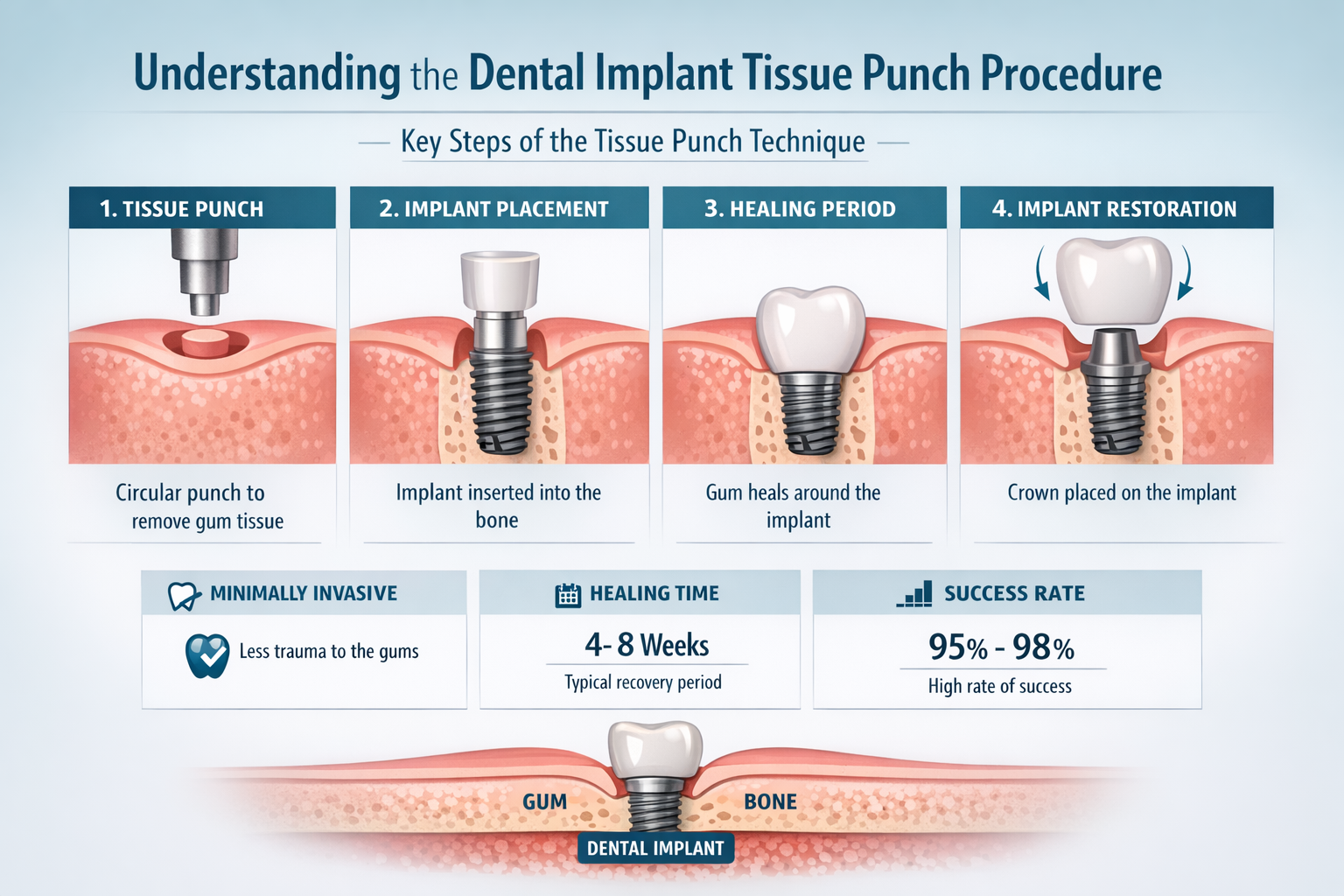
- What is a Tissue Punch? A tissue punch is a precise technique used to create a circular opening in the gum tissue, allowing access for dental implant placement or exposure without needing a large surgical flap, often leading to less trauma and faster initial healing.
- Phases of Healing: Dental implant tissue punch healing progresses through inflammatory, proliferative (granulation tissue formation), and remodeling phases, each crucial for soft tissue integration and health around the implant.
- Factors Influencing Healing: Several factors impact healing, including surgical technique, patient’s overall health, oral hygiene, smoking status, and proper post-operative care.
- Recognizing Complications: While generally smooth, it’s essential to identify signs of complications such as persistent pain, swelling, pus, or implant mobility, and contact your dental professional immediately.
- Optimal Post-Operative Care: Diligent oral hygiene, adherence to dietary restrictions (like those found in 50 Soft Foods After Dental Implant), and avoiding smoking are paramount for successful dental implant tissue punch healing.
Understanding the Dental Implant Tissue Punch Procedure
The tissue punch technique is a surgical method employed during dental implant placement, particularly in a two-stage implant protocol or for uncovering implants previously placed beneath the gum line. Instead of using a traditional scalpel incision and lifting a gum flap, a specialized circular instrument—the tissue punch—is used to remove a small, precise disc of gum tissue [1]. This creates a clean opening, exposing the underlying bone for implant placement or revealing the top of a buried implant for abutment connection.
Why Choose a Tissue Punch?
The primary advantages of using a tissue punch over a traditional flap surgery include:
- Minimally Invasive: It involves less trauma to the surrounding tissues, as a smaller amount of tissue is disturbed.
- Reduced Bleeding and Swelling: Less tissue manipulation often translates to less post-operative bleeding and swelling.
- Faster Initial Healing: The localized nature of the punch can lead to quicker initial soft tissue closure and comfort.
- Preservation of Keratinized Gingiva: In some cases, it can help preserve the valuable keratinized tissue around the implant, which is crucial for long-term gum health and stability.
- Improved Aesthetics: A precise punch can contribute to a more natural and aesthetic gum contour around the final crown.
However, it’s important to note that the tissue punch technique is not suitable for all cases. It requires sufficient attached gingiva and is typically used when no bone grafting or significant soft tissue contouring is needed [2]. Your dental surgeon will determine the most appropriate technique based on your individual anatomical considerations and treatment plan. To learn more about various implant procedures, explore our About Us page.
The Role of Tissue Punch in Dental Implant Placement
When a dental implant is initially placed, it might be entirely covered by gum tissue (a two-stage approach) to allow for undisturbed healing and osseointegration—the fusion of the implant with the bone. After a period, typically several months, a second minor surgical procedure is performed to expose the implant. This is where the tissue punch often comes into play. The punch precisely removes the tissue covering the implant, allowing the placement of a healing abutment. This abutment then shapes the gum tissue around the implant, preparing it for the final crown. Understanding this step is crucial for comprehending the nuances of dental implant tissue punch healing.
The Stages of Dental Implant Tissue Punch Healing
The process of dental implant tissue punch healing is a marvel of biological regeneration. Like any wound healing, it progresses through several predictable stages, each vital for the successful integration and long-term health of the implant site.
1. The Inflammatory Phase (Days 1-3)
Immediately after the tissue punch procedure, the body initiates its natural healing response. This phase is characterized by:
- Hemostasis: Blood vessels constrict to limit bleeding, and platelets aggregate to form a clot, sealing the wound.
- Inflammation: Immune cells, such as neutrophils and macrophages, rush to the site to clean up debris, bacteria, and damaged tissue.
- Symptoms: Patients may experience mild swelling, redness, and discomfort, which are normal signs of the body’s healing mechanism. This phase is critical for preparing the wound bed for subsequent repair.
- Clinical Appearance: The area may appear slightly red and swollen, with a thin fibrin clot covering the punched site.
2. The Proliferative Phase (Days 3-21)
Following the initial inflammation, the body moves into the proliferative phase, focusing on rebuilding tissue.
- Granulation Tissue Formation: Fibroblasts migrate into the wound, laying down new collagen fibers, and new blood vessels (angiogenesis) form to supply nutrients. This combination forms granulation tissue, which looks red and granular.
- Epithelialization: Epithelial cells from the edges of the wound begin to migrate and cover the exposed surface, gradually closing the defect created by the punch. This process is key for soft tissue closure.
- Tissue Maturation: As epithelialization progresses, the initial wound begins to shrink, and the new soft tissue starts to gain strength and organization around the healing abutment.
- Clinical Appearance: The redness and swelling subside, and the tissue around the implant begins to look healthier and more contoured, adapting to the shape of the healing abutment. This is a critical period for proper dental implant tissue punch healing.
3. The Remodeling Phase (Weeks 3 Onwards)
This is the longest phase, where the newly formed tissue matures and strengthens.
- Collagen Remodeling: The disorganized collagen fibers laid down in the proliferative phase are reorganized, strengthened, and cross-linked, increasing the tensile strength of the tissue.
- Vascular Maturation: Blood vessels mature and regress as needed, optimizing blood supply to the healed tissue.
- Functional Adaptation: The soft tissue surrounding the implant adapts to its new function, forming a tight seal around the healing abutment, which is crucial for protecting the implant from bacterial invasion.
- Clinical Appearance: The gum tissue attains its final, healthy appearance—firm, pink, and well-adapted around the healing abutment, ready for the definitive abutment and crown placement. You can learn more about this process in our guide on abutment placement.
It’s important to remember that while these stages are distinct, they often overlap. The entire process of soft tissue healing around a dental implant can take several weeks to a few months to reach full maturity, even if the initial discomfort subsides quickly.
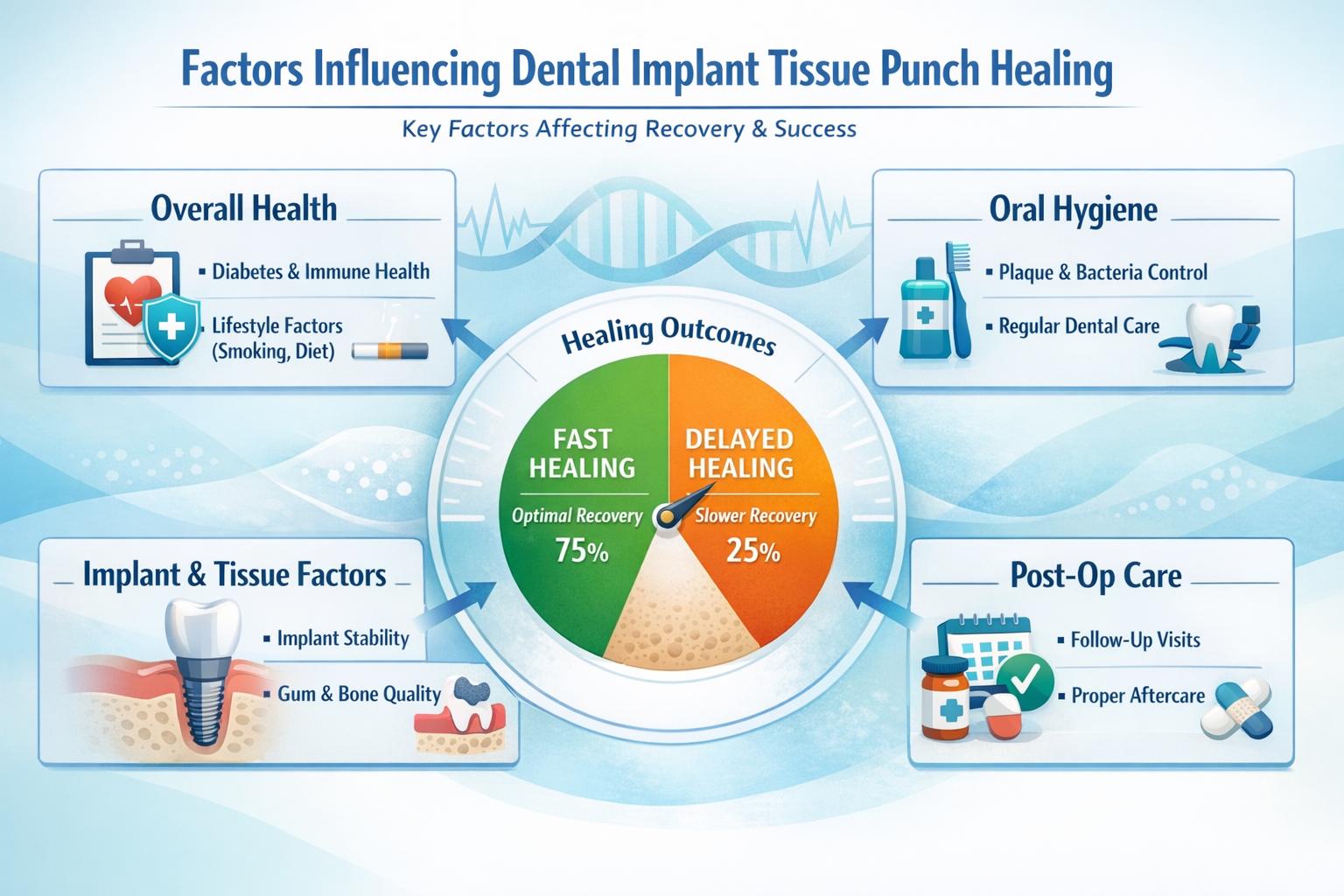
Factors Influencing Dental Implant Tissue Punch Healing
The success and speed of dental implant tissue punch healing are not solely dependent on the surgical technique but are also significantly influenced by a variety of patient-specific and procedural factors. Understanding these elements can empower patients to take an active role in optimizing their recovery.
Patient-Related Factors
- Overall Health Status: Patients with well-controlled systemic conditions, such as diabetes, tend to heal more predictably than those with poorly managed conditions [3]. A healthy immune system is vital for effective wound repair.
- Smoking: Smoking is a well-documented deterrent to healing. Nicotine constricts blood vessels, reducing blood flow and oxygen delivery to the surgical site, thereby delaying healing and increasing the risk of complications like infection and implant failure [4]. Patients are strongly advised to cease smoking before and after dental implant procedures.
- Nutrition: Adequate nutrition, particularly sufficient intake of vitamins (especially C and D) and protein, provides the building blocks for tissue repair and immune function.
- Age: While older individuals may have a slightly slower metabolic rate, age itself is not a contraindication for dental implants. Healthy older adults can achieve excellent healing outcomes.
- Oral Hygiene: Pre-existing poor oral hygiene can increase the bacterial load in the mouth, raising the risk of infection at the surgical site. Good oral hygiene is paramount throughout the entire implant process.
Surgical and Post-Operative Factors
Surgical Technique: The precision and atraumatic nature of the tissue punch procedure itself play a significant role. A skilled surgeon minimizes tissue damage, which contributes to faster, more predictable healing.
Primary Stability of Implant: While the tissue punch primarily affects soft tissue, the underlying bone healing and implant stability are interconnected. A well-integrated implant provides a stable foundation for the surrounding soft tissue.
Healing Abutment Design: The shape and size of the healing abutment can influence the contouring of the gum tissue as it heals around the implant. Proper selection ensures optimal aesthetic and functional outcomes.
Post-Operative Care: Adherence to post-operative instructions is critical. This includes:
- Medication: Taking prescribed antibiotics and pain relievers as directed.
- Diet: Sticking to soft foods initially (refer to 50 Soft Foods After Dental Implant) to avoid disrupting the healing site.
- Oral Hygiene: Gentle cleaning around the surgical site, as instructed by the dental professional.
- Avoiding Habits: Refraining from smoking, alcohol, and using straws (which can dislodge blood clots). More detailed information can be found in our article on alcohol after dental implant surgery.
Infection Control: Strict infection control during and after surgery is vital. Any signs of infection (pus, fever, worsening pain) should be reported immediately.
By understanding and managing these influencing factors, patients can significantly contribute to the success of their dental implant tissue punch healing.
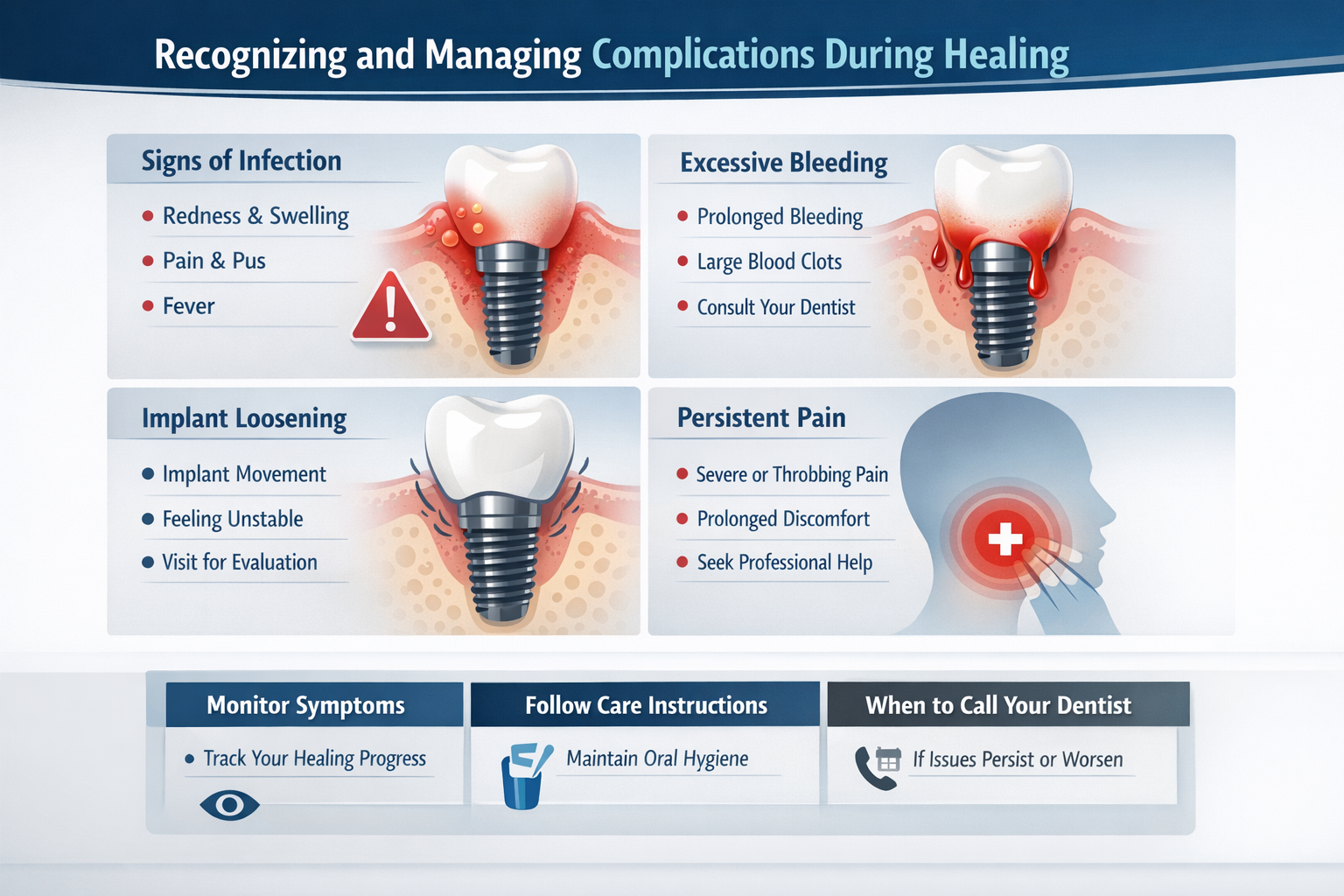
Recognizing and Managing Complications During Healing
While dental implant tissue punch healing is generally smooth, it’s essential for patients to be aware of potential complications. Early recognition and intervention are key to successful management and preventing more serious issues.
Common Signs of Normal Healing vs. Concern
It’s crucial to differentiate between normal post-operative symptoms and signs that may indicate a complication.
| Symptom | Normal Healing (Expectations) | Potential Complication (Call Your Dentist) |
|---|---|---|
| Pain | Mild discomfort, manageable with over-the-counter pain relievers, gradually decreasing over a few days. | Severe or worsening pain that isn’t relieved by medication, throbbing pain. |
| Swelling | Mild to moderate swelling for 2-3 days, gradually subsiding. | Persistent or increasing swelling after 3-4 days, accompanied by fever. |
| Bleeding | Slight oozing or pink saliva for the first 24-48 hours. | Heavy or continuous bleeding that doesn’t stop with gentle pressure. |
| Bruising | Possible mild bruising on the skin, especially for larger procedures. | Extensive bruising spreading beyond the immediate area. |
| Taste/Odor | None or minimal change. | Persistent bad taste in the mouth or foul odor from the implant site. |
| Pus/Discharge | None. | Yellow, green, or white discharge (pus) from the surgical site. |
| Fever | None or very low grade, temporary. | High fever (over 100.4°F or 38°C). |
| Implant Mobility | Implant should be firm and stable. | Any noticeable movement or wobbling of the healing abutment or implant itself. |
Potential Complications and Their Management
- Infection (Peri-implantitis): This is the most common concern. Symptoms include persistent pain, swelling, redness, pus discharge, and potentially fever. If an infection is suspected, your dentist will likely prescribe antibiotics and may need to clean the site thoroughly. Early detection of dental implant bleeding or pus is critical.
- Delayed Healing: If the tissue doesn’t seem to be closing or maturing as expected, it could be due to factors like smoking, poor nutrition, or underlying systemic issues. Your dentist may offer advice on improving healing conditions.
- Healing Abutment Dislodgement: While rare, the healing abutment might loosen or fall out. If this happens, contact your dental office immediately. It usually needs to be re-seated or replaced to guide proper tissue formation.
- Tissue Overgrowth: Sometimes, the gum tissue might grow over the healing abutment. This typically requires a minor adjustment by your dentist to re-expose the abutment.
- Allergic Reaction: Although uncommon with titanium implants, some individuals may react to materials. Symptoms could include persistent redness, itching, or swelling.
- Implant Failure: In rare cases, the implant may not successfully integrate with the bone (osseointegration failure). This can sometimes manifest during the soft tissue healing phase if the implant feels loose. If the implant fails, it may need to be removed and, after further healing, a new implant placed. For more information, refer to our comprehensive guide on complete dental implant recovery timeline.
“Early detection and communication with your dental professional are the cornerstones of managing any complications during dental implant tissue punch healing. Do not hesitate to report any unusual or worsening symptoms.”
Regular follow-up appointments are crucial during the healing period. Your dental professional will monitor your progress and address any concerns proactively, ensuring the best possible outcome for your dental implant.
Optimal Post-Operative Care for Enhanced Tissue Punch Healing
Achieving successful dental implant tissue punch healing relies heavily on diligent post-operative care. By following your dental professional’s instructions meticulously, you can minimize complications, promote rapid healing, and ensure the longevity of your dental implant.
Immediate Post-Operative Care (First 24-48 Hours)
- Manage Bleeding: Slight oozing is normal. Bite gently on a sterile gauze pad placed over the surgical site for 30-60 minutes, replacing it as needed. Avoid vigorous rinsing or spitting, which can dislodge the blood clot.
- Control Swelling: Apply an ice pack to the outside of your cheek, near the surgical site, for 20 minutes on, 20 minutes off, for the first 24-48 hours. This helps reduce swelling and discomfort.
- Pain Management: Take prescribed pain medication as directed. Over-the-counter anti-inflammatory drugs like ibuprofen can also be very effective.
- Rest: Get plenty of rest. Avoid strenuous activities for at least the first 24-48 hours.
- Dietary Restrictions: Stick to soft, cool foods and liquids. Avoid hot liquids, spicy foods, crunchy items, and anything that requires significant chewing. Consult our guide on 50 Soft Foods After Dental Implant for ideas.
- Oral Hygiene: Do NOT rinse your mouth vigorously or brush the surgical site directly for the first 24 hours. After 24 hours, gentle rinsing with a prescribed antimicrobial mouthwash or warm salt water (1/2 teaspoon salt in 8 ounces of warm water) can begin, up to 2-3 times a day.
- Avoid Smoking and Alcohol: Both smoking and alcohol can severely impede healing. Refrain from these completely for as long as possible, ideally for the entire healing period. For more details, see our article on alcohol after dental implant surgery.
Ongoing Care (Beyond 48 Hours to Full Healing)
- Gentle Oral Hygiene: Continue gentle brushing around the healing abutment with a soft-bristled toothbrush. Your dental professional may recommend specific techniques or interdental brushes. Do not aggressively pick or probe the healing site.
- Medication Adherence: Finish any prescribed antibiotics, even if you feel better, to prevent infection.
- Diet Progression: Gradually reintroduce solid foods as comfort allows, but continue to avoid extremely hard, sticky, or crunchy foods directly at the implant site until fully healed.
- Avoid Trauma: Be careful not to bump or disturb the healing abutment. Avoid habits like nail-biting or chewing on pens.
- Follow-up Appointments: Attend all scheduled follow-up appointments. These visits allow your dental professional to monitor your healing progress and ensure everything is on track.
- Stay Hydrated: Drink plenty of water to aid overall bodily functions and healing.
Long-Term Maintenance for Implant Health
Even after the initial soft tissue healing, ongoing commitment to oral hygiene is crucial for the long-term success of your dental implant.
- Regular Brushing and Flossing: Treat your dental implant like your natural teeth. Brush twice daily and floss (or use an interdental cleaner) daily.
- Professional Cleanings: Schedule regular dental check-ups and professional cleanings, typically every six months. Inform your hygienist that you have dental implants so they can use appropriate tools and techniques for cleaning around them. More information on cleaning costs can be found on our dental implant cleaning cost page.
- Monitor for Changes: Pay attention to any changes around your implant, such as redness, swelling, or bleeding, and report them to your dentist promptly.
By diligently following these guidelines, you significantly contribute to a healthy and successful dental implant tissue punch healing outcome, paving the way for a stable and beautiful new smile. For general information about dental implants, visit https://dentalimplantsdallastx.com/.
Interactive Tool: Dental Implant Tissue Punch Healing Timeline
This interactive timeline helps visualize the typical healing progression after a dental implant tissue punch procedure. Select a time point to see the expected symptoms and care instructions.
Day 1: Initial Response (Inflammatory Phase)
- Symptoms: Mild pain, slight swelling, minimal bleeding/oozing, may see a blood clot.
- Care: Gentle bite on gauze (30-60 min), ice pack (20 min on/off), take prescribed pain meds. Soft, cool diet. No rinsing, spitting, or brushing surgical site. Avoid smoking/alcohol.
- Goal: Control bleeding, minimize swelling, and initiate clotting.
Conclusion
The journey of dental implant tissue punch healing is a finely orchestrated biological process that lays the groundwork for the long-term success and aesthetic appeal of your dental implant. From the initial inflammatory response to the final remodeling of soft tissue, each stage is critical. Understanding this process empowers patients to actively participate in their recovery and appreciate the meticulous care involved in modern implant dentistry.
Optimal healing is a collaborative effort between the patient and the dental team. By adhering to post-operative instructions, maintaining impeccable oral hygiene, and promptly communicating any concerns, patients significantly enhance their healing outcomes. The reward is a healthy, stable, and aesthetically pleasing gum tissue contour around the implant, which is vital for protecting the underlying bone and ensuring the longevity of your new smile.
As dental technology and techniques continue to evolve in 2026, the emphasis remains on minimally invasive procedures and patient-centered care. The tissue punch technique exemplifies this approach by facilitating efficient and comfortable soft tissue management around dental implants.
Actionable Next Steps:
- Follow Instructions Diligently: Re-read and strictly follow all post-operative instructions provided by your dental professional. Do not hesitate to ask clarifying questions.
- Maintain Oral Hygiene: Gently clean the surgical site as instructed. Regular, gentle oral care is paramount.
- Monitor Your Healing: Be aware of the normal signs of healing and learn to identify potential complications. Use the interactive timeline provided to understand what to expect.
- Attend Follow-up Appointments: These are crucial for your dental team to monitor your progress and ensure optimal dental implant tissue punch healing.
- Avoid Detrimental Habits: Refrain from smoking, excessive alcohol consumption, and any activities that could disturb the healing site.
By taking these steps, you are actively investing in the health and success of your dental implant, paving the way for a beautiful and functional restoration for many years to come. For specific questions or to schedule a consultation, visit https://dentalimplantsdallastx.com/contact-us/.
References
[1] Misch, C. E. (2014). Dental Implant Prosthetics (2nd ed.). Mosby Elsevier.
[2] Buser, D., Belser, U. C., & Wismeijer, D. (Eds.). (2017). ITi Treatment Guide Vol. 10: Digital Workflow in Implant Dentistry. Quintessence Publishing.
[3] Chrcanovic, B. R., Albrektsson, T., & Wennerberg, A. (2014). Diabetes and oral implant failure: a systematic review. Journal of Dental Research, 93(6), 522-527.
[4] Quirynen, M., De Soete, M., & van Steenberghe, D. (2000). Infectious risks for oral implants: a review of the literature. Clinical Oral Implants Research, 11(1), 1-19.

Leave a Reply
Share your thoughts or ask a question about dental implants. Your email address will not be published.