Undergoing a dental implant procedure is a significant step towards restoring your smile and oral health. It’s natural to feel a mix of excitement and apprehension. One common concern that often arises after the surgery is the presence of blood. If you find yourself spitting blood after dental implant placement, you’re not alone in wondering if this is a normal part of the healing process or a cause for alarm. As an expert SEO content strategist and senior editor, I’m here to guide you through what to expect, when to be concerned, and how to manage this common post-operative occurrence in 2026.
Key Takeaways
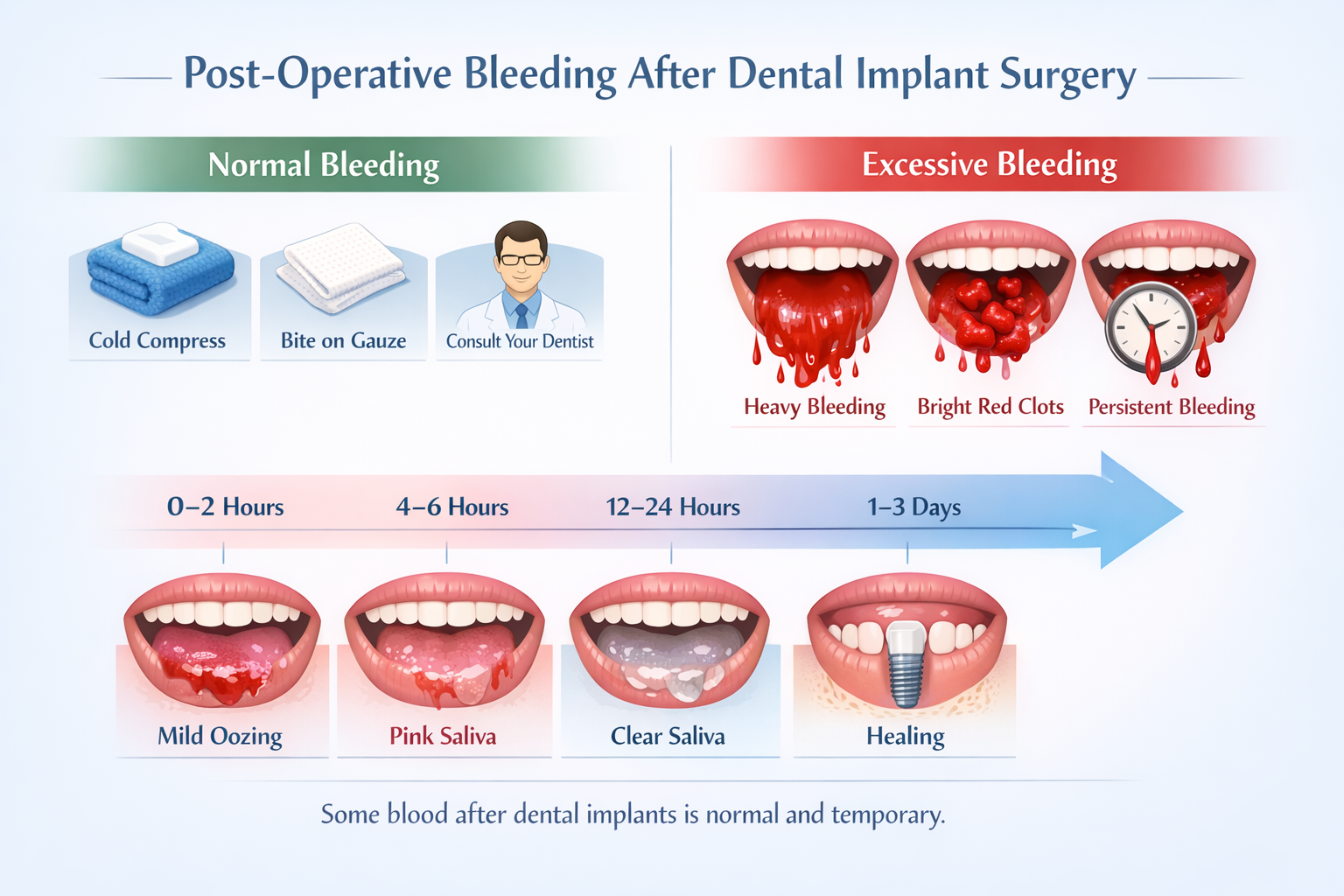
- Normal vs. Abnormal Bleeding: A small amount of oozing or pink-tinged saliva is normal for the first 24-48 hours after dental implant surgery. Heavy, bright red bleeding or large clots are not.
- Initial Management: Apply firm, consistent pressure with a sterile gauze pad for 30-60 minutes to control minor bleeding.
- Oral Hygiene: Gentle oral care is crucial, but avoid rinsing vigorously, spitting, or using straws, as these can dislodge blood clots and restart bleeding.
- Dietary Adjustments: Stick to soft foods and avoid hot beverages immediately after surgery to prevent irritating the surgical site. Check out our guide on 50 Soft Foods After Dental Implant for more ideas.
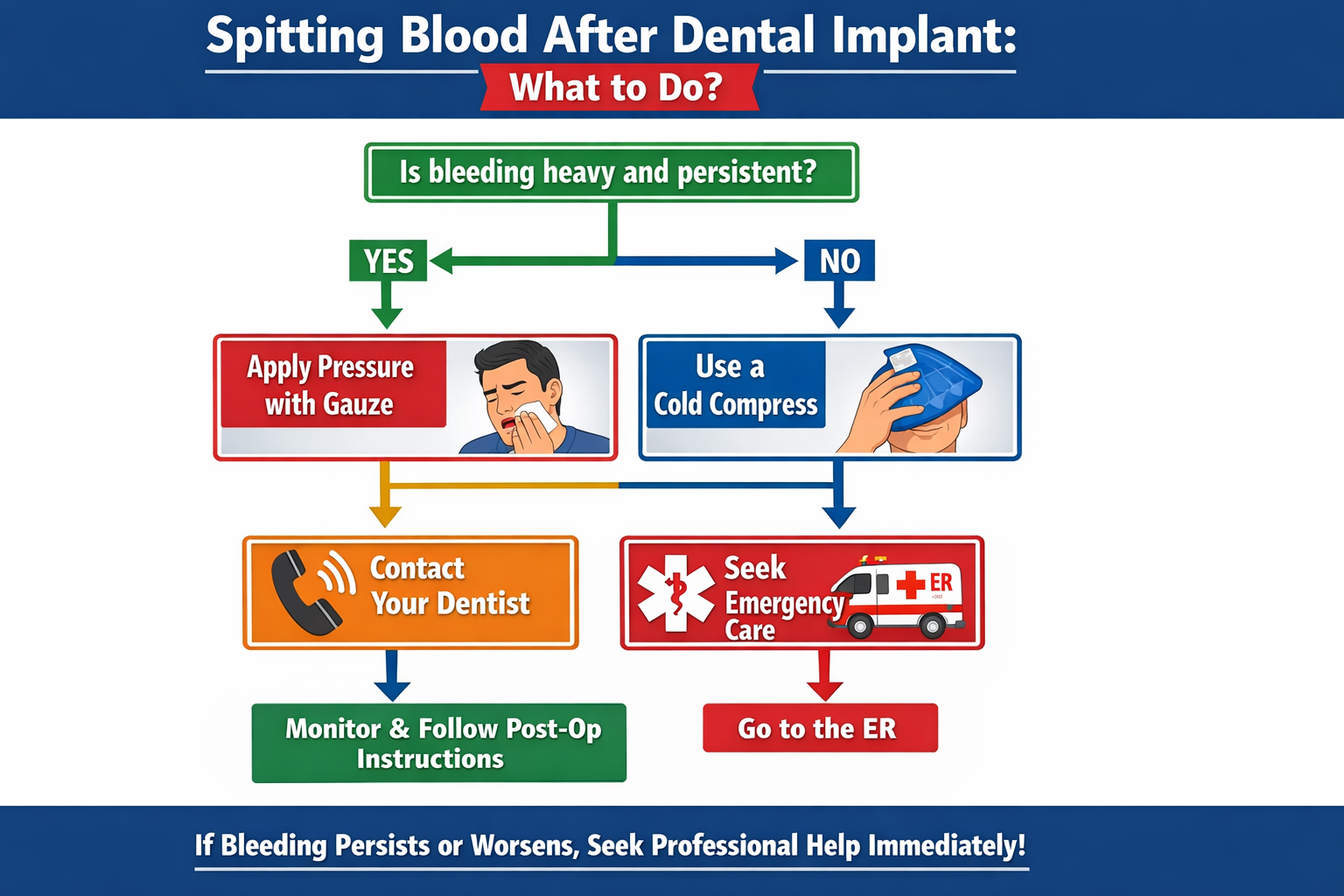
- When to Contact Your Dentist: If bleeding is heavy, persistent, or accompanied by severe pain, swelling, or fever, contact your dental professional immediately.
Understanding Post-Operative Bleeding: Is Spitting Blood After Dental Implant Normal?
After any surgical procedure, a certain degree of bleeding is to be expected. Dental implant surgery is no exception. The delicate tissues of your mouth are highly vascular, meaning they have a rich blood supply. When incisions are made and an implant is placed into the jawbone, blood vessels are inevitably affected. So, is spitting blood after dental implant a normal occurrence? Generally, yes, to a certain extent.
The First 24-48 Hours: What to Expect
In the immediate hours following your dental implant procedure, it is entirely normal to experience some oozing or a slight reddish discoloration of your saliva. This is often described as “pink-tinged saliva” or “light bleeding” and should gradually subside. Your body is forming a blood clot at the surgical site, which is a crucial first step in the healing process.
Think of it like a minor cut on your finger – it might bleed for a bit, but then a scab forms. In your mouth, that “scab” is a delicate blood clot. Any disruptive actions, such as vigorous rinsing or spitting, can dislodge this clot, leading to renewed bleeding. This is why your dentist will provide very specific post-operative instructions, emphasizing gentle care.
Table: Expected Bleeding Levels After Dental Implant Surgery
| Timeframe After Surgery | Expected Bleeding Level | Action/Observation |
|---|---|---|
| 0-4 hours | Moderate oozing, pink or reddish saliva | Keep gauze in place with firm pressure. Change as needed. |
| 4-24 hours | Light oozing, pink-tinged saliva, possibly small clots | Continue gentle care. Avoid vigorous activities. Minimal bleeding is normal. |
| 24-48 hours | Very light pink saliva, minimal to no active bleeding | Bleeding should be significantly reduced or stopped. Contact dentist if persistent heavy bleeding. |
| 48+ hours | No active bleeding, clear saliva | Healing should be well underway. Minor discoloration from food or drinks is normal, but not blood. |
It’s crucial to remember that this table outlines general expectations. Individual experiences may vary. Always follow your dentist’s specific instructions.
Why Does Bleeding Occur?
The primary reasons for post-operative bleeding include:
- Tissue Trauma: Any surgical incision causes trauma to the blood vessels in the surrounding gum tissue and bone.
- Capillary Leakage: Even after the main bleeding is controlled, small capillaries can continue to leak blood and plasma, contributing to the discoloration of saliva.
- Dislodged Blood Clot: This is a common culprit for renewed bleeding. If the blood clot that forms over the surgical site is disturbed by actions like forceful spitting, rinsing, or even eating hard foods, the bleeding can restart. This condition is sometimes referred to as a “dry socket” if the clot is lost entirely, which can be quite painful and delay healing.
- Underlying Medical Conditions: In rare cases, certain medical conditions (like bleeding disorders) or medications (like blood thinners) can increase the risk of prolonged bleeding. Always inform your dentist about your full medical history and all medications you are taking.
Understanding these factors can help alleviate some anxiety when you notice spitting blood after dental implant surgery. Knowing what’s normal allows you to focus on proper aftercare and recognize when to seek professional advice. For a deeper dive into overall recovery, you might find our article on the complete dental implant recovery timeline helpful.
When to Be Concerned About Spitting Blood After Dental Implant
While some bleeding is normal, it’s vital to differentiate between minor oozing and excessive or prolonged bleeding. Recognizing the signs of an issue can help you act quickly and prevent complications.
Signs of Excessive or Abnormal Bleeding
You should be concerned and contact your dentist if you experience any of the following:
- Heavy, Continuous Bleeding: If you are consistently spitting out mouthfuls of bright red blood, or if the bleeding doesn’t slow down after applying pressure for 30-60 minutes, this is a sign that something might be amiss.
- Large Blood Clots: While small, jelly-like clots are common, very large, golf-ball-sized clots, or a continuous formation of large clots, warrant attention.
- Bleeding that Worsens After 48 Hours: Bleeding should be diminishing, not increasing, after the initial 1-2 days. If you’re still experiencing significant spitting blood after dental implant placement beyond this period, contact your dental team.
- Bleeding Accompanied by Other Symptoms:
- Severe or increasing pain: Pain that isn’t managed by prescribed pain medication or worsens significantly.
- Excessive swelling or bruising: While some swelling is normal, rapid or extreme swelling might indicate a problem.
- Fever: A fever can be a sign of infection.
- Difficulty swallowing or breathing: This is a rare but serious symptom that requires immediate medical attention.
“While some blood-tinged saliva is expected, if you’re consistently filling your mouth with bright red blood or experiencing large clots, it’s time to reach out to your dental professional.”
Immediate Steps to Take if Bleeding is Excessive
If you suspect you’re experiencing more than normal bleeding, take these immediate steps:
- Apply Firm Pressure with Gauze:
- Fold a piece of sterile gauze into a thick pad and place it directly over the surgical site.
- Bite down firmly on the gauze for at least 30-60 minutes. The pressure is key to stopping the bleeding.
- Avoid checking the gauze too frequently, as this can disrupt the forming clot.
- If the gauze becomes saturated, replace it with a fresh piece and continue applying pressure. You may need to repeat this process several times.
- Use a Cold Compress:
- Apply an ice pack or a bag of frozen peas wrapped in a cloth to the outside of your cheek, near the surgical area.
- Apply for 15-20 minutes, then remove for 15-20 minutes. Repeat this cycle for several hours. This helps to constrict blood vessels and reduce swelling and bleeding.
- Elevate Your Head:
- When resting or sleeping, keep your head elevated with extra pillows. This can help reduce blood flow to the head and minimize bleeding.
- Avoid Irritating Activities:
- Do NOT rinse your mouth vigorously.
- Do NOT spit. Swallowing small amounts of blood-tinged saliva is acceptable.
- Do NOT use a straw. The suction can dislodge the blood clot.
- Avoid smoking or consuming alcohol. Both can impede healing and increase bleeding. Learn more about alcohol after dental implant surgery.
- Avoid hot liquids and hard, crunchy, or spicy foods. Stick to soft, cool foods. We have an excellent list of soft foods after dental implant options that can help.
- Contact Your Dentist:
- If bleeding persists and remains heavy despite applying pressure for an hour or more, or if you have any other concerning symptoms, call your dentist’s office immediately. They will provide specific advice or ask you to come in for an evaluation. If it’s outside of office hours, they usually have an emergency contact number.
It’s better to err on the side of caution. Your dental implant provider is the best resource for guidance if you are concerned about spitting blood after dental implant surgery. Don’t hesitate to reach out to them.
Post-Operative Care Strategies to Minimize Bleeding and Promote Healing
Proper post-operative care is paramount not only to minimize bleeding but also to ensure the successful integration of your dental implant with your jawbone, a process known as osseointegration. Following your dentist’s instructions meticulously is the best way to promote a smooth recovery.
The Role of Gauze and Pressure
As mentioned, applying firm, consistent pressure with sterile gauze is your first line of defense against post-operative bleeding. The goal is to allow a stable blood clot to form.
- How to apply: Fold 2-3 pieces of gauze into a small, thick pad. Place it directly over the surgical site and bite down firmly. The pressure should be enough to hold the gauze in place and compress the wound.
- Duration: Maintain pressure for 30-60 minutes without removal. If bleeding continues, replace with new gauze and reapply pressure for another 30-60 minutes.
- Avoid “Tea Bags” unless directed: Some older advice suggests using tea bags (especially black tea due to tannic acid). While tannic acid can aid in coagulation, it’s generally best to stick to sterile gauze unless explicitly advised by your dentist.
Gentle Oral Hygiene Practices
Maintaining oral hygiene is critical to prevent infection, but it must be done gently to avoid disturbing the healing site.
- Avoid Rinsing for the First 24 Hours: Do not rinse your mouth at all for the first 24 hours after surgery. This is critical to allow the blood clot to stabilize.
- Gentle Rinsing After 24 Hours: After the first 24 hours, you can gently rinse with a warm salt water solution (1/2 teaspoon of salt in 8 ounces of warm water) 2-3 times a day. Do not swish vigorously. Instead, let the water gently “bathe” the area and then allow it to spill out of your mouth rather than spitting.
- Brushing: You can brush your teeth gently, but avoid brushing directly on or near the surgical site for several days. Use a soft-bristled toothbrush.
- Prescribed Mouthwash: Your dentist might prescribe a special antiseptic mouthwash (like chlorhexidine gluconate). Use this exactly as directed, being careful not to rinse forcefully.
- Avoid Electric Toothbrushes and Water Flossers: For the initial healing phase, these can be too aggressive and dislodge clots. Check with your dentist about when it’s safe to resume using a water flosser, as these can be great for long-term implant care. For optimal long-term care, see our guide on the best water flosser for dental implants.
Dietary Considerations
What you eat and drink can significantly impact your recovery and bleeding.
- Soft Foods: Stick to a diet of soft, non-chewy foods for the first few days. Examples include yogurt, mashed potatoes, scrambled eggs, smoothies (without a straw!), and soups (lukewarm, not hot). Our 50 Soft Foods After Dental Implant article offers extensive suggestions.
- Avoid Hot Beverages: Heat can increase blood flow and potentially dislodge clots. Let coffee, tea, and other hot drinks cool down.
- No Straws: The suction created by using a straw can pull on the blood clot and dislodge it, leading to renewed bleeding.
- Hydration: Drink plenty of fluids (water, fruit juices, milk), but avoid carbonated beverages or those with a high sugar content.
Pain Management and Medications
Your dentist will likely prescribe pain medication and possibly antibiotics to manage discomfort and prevent infection.
- Pain Relievers: Take prescribed pain medication as directed. Over-the-counter options like ibuprofen can also help reduce pain and inflammation.
- Antibiotics: If prescribed, take the full course of antibiotics, even if you start feeling better. This is crucial for preventing infection, which can complicate healing and potentially lead to bleeding. Read more about antibiotics after dental implant surgery.
- Anti-Inflammatory Drugs: Some medications can help reduce swelling, which indirectly aids in controlling bleeding.
Lifestyle Adjustments
- Rest: Get plenty of rest. Avoid strenuous physical activity for at least the first 48-72 hours, as this can increase blood pressure and restart bleeding.
- No Smoking: Smoking severely impedes healing and increases the risk of complications, including prolonged bleeding and implant failure. If you smoke, this is the best time to consider quitting. You can learn more about concerns like after root canal can you smoke for similar dental procedures.
- Avoid Alcohol: Alcohol can thin the blood and interfere with medications. Avoid it during your recovery.
- Follow-Up Appointments: Attend all scheduled follow-up appointments with your dentist. These are vital for monitoring your healing progress and addressing any concerns.
By diligently following these post-operative care instructions, you significantly increase your chances of a smooth recovery with minimal issues, including effectively managing any spitting blood after dental implant procedures.
Potential Complications Associated with Excessive Bleeding
While minor spitting blood after dental implant is often benign, uncontrolled or prolonged bleeding can lead to several complications. Being aware of these can help you understand the importance of proper care and timely professional intervention.
Delayed Healing
The formation of a stable blood clot is the initial and most critical step in wound healing. If this clot is continually dislodged or if bleeding is persistent, it can delay the entire healing process. The body struggles to lay down new tissue and bone when constantly fighting active bleeding, which can impact the crucial osseointegration process where the implant fuses with the jawbone.
Increased Risk of Infection
Blood is a rich nutrient source for bacteria. Persistent bleeding can create a favorable environment for bacterial growth around the surgical site, increasing the risk of post-operative infection. An infected site can lead to:
- Pain and Swelling: Worsening discomfort and noticeable swelling.
- Pus Formation: Discharge from the surgical area.
- Fever: A systemic sign of infection.
- Implant Failure: In severe cases, an infection can lead to the failure of the dental implant, necessitating its removal. This is a significant concern for any patient seeking to replace missing teeth.
Anemia
While rare from dental implant surgery alone, very prolonged and heavy bleeding can, in extreme cases, contribute to anemia, especially in individuals who are already predisposed. Anemia can lead to fatigue, weakness, and other systemic health issues.
Hematoma Formation
Excessive bleeding can sometimes lead to the formation of a hematoma – a localized collection of blood outside of blood vessels, often clotted. This can present as a firm, swollen, bruised area. While many hematomas resolve on their own, large ones can cause discomfort, pressure, and potentially delay healing or increase the risk of infection.
Disruption of Osseointegration
The success of a dental implant hinges on its ability to integrate with the surrounding jawbone. This process, known as osseointegration, requires a stable, undisturbed healing environment. Persistent bleeding or the repeated loss of the blood clot can disrupt this delicate process, potentially leading to the implant failing to fuse properly with the bone. This could necessitate the removal of the implant and, in some cases, further bone grafting before another attempt can be made. This is a critical concern, especially for those who have experienced issues like 90 percent bone loss in teeth and required significant preparation for their implants.
Psychological Distress
Beyond the physical complications, persistent or heavy spitting blood after dental implant surgery can cause significant anxiety and distress for the patient. Worrying about one’s health and the success of the procedure can be emotionally draining. This stress can, in turn, impede the healing process.
By diligently following your dentist’s post-operative instructions and being vigilant about any signs of excessive bleeding, you can minimize the risk of these potential complications and ensure a smoother, more successful recovery.
Long-Term Healing and Maintenance for Your Dental Implant
After the initial post-operative period where spitting blood after dental implant becomes a non-issue, the journey to full healing and successful implant longevity continues. Dental implants require ongoing care and attention, just like your natural teeth, to ensure their success for many years to come.
The Osseointegration Period
The most critical long-term healing phase is osseointegration. This is the biological process where the dental implant, typically made of titanium, fuses directly with your jawbone. This process can take anywhere from 3 to 6 months, sometimes longer, depending on individual healing capabilities, bone density, and the specific implant type (e.g., immediate load vs. traditional).
During this time, it’s crucial to:
- Avoid Pressure on the Implant Site: If you have a temporary crown or denture, be cautious not to put excessive chewing pressure directly on the healing implant.
- Maintain Excellent Oral Hygiene: Continue with the gentle oral hygiene practices recommended by your dentist. Preventing infection during this phase is paramount for successful osseointegration.
- Attend Follow-Up Appointments: Your dentist will want to monitor the healing process, often using X-rays, to ensure the implant is properly fusing with the bone.
Abutment Placement and Crown Restoration
Once osseointegration is complete, the next step usually involves the placement of the abutment – a small connector post that attaches to the implant and protrudes through the gum line. This step often requires a minor surgical procedure. After the gums heal around the abutment (typically 1-2 weeks), your permanent crown, bridge, or denture will be fabricated and attached. This completes the restoration, allowing you to chew and speak normally. You can learn more about this crucial stage in our guide to the complete guide to the dental implant abutment procedure.
Lifelong Maintenance of Your Dental Implants
Even after your implant is fully restored, it requires diligent care for its entire lifespan.
- Regular Brushing and Flossing: Treat your dental implant like your natural teeth. Brush at least twice a day and floss daily. Special floss designed for implants or interdental brushes may be recommended to clean around the implant post.
- Specialized Oral Hygiene Tools: Many dentists recommend a water flosser for cleaning around implants, as it can effectively remove plaque and food debris from hard-to-reach areas without being too abrasive. Refer to our recommendations for the best water flosser for dental implants.
- Dental Check-ups and Cleanings: Regular visits to your dentist and hygienist (typically every 6 months) are essential. Hygienists have specialized tools to clean around implants without scratching the titanium surface. They can also monitor the health of your gums and surrounding bone.
- Avoid Harmful Habits: Refrain from biting on hard objects (ice, pens), grinding your teeth (bruxism), or using your teeth as tools, as these can damage your implant crown or even the implant itself. If you clench or grind, discuss this with your dentist, as a night guard may be recommended.
- Address Issues Promptly: If you notice any redness, swelling, bleeding (beyond the initial post-op phase), or discomfort around your implant, contact your dentist immediately. Early intervention can prevent serious issues like peri-implantitis (gum disease affecting implants).
By committing to these long-term care strategies, you can ensure your dental implant remains a healthy, functional, and aesthetic part of your smile for decades. For more comprehensive information on dental implants and their care, feel free to visit our main site at Dental Implants Dallas TX.
Conclusion
The journey to a restored smile with dental implants is a remarkable one, offering unparalleled benefits in terms of function, aesthetics, and confidence. Experiencing spitting blood after dental implant surgery is a common and often normal part of the initial healing phase. By understanding what to expect – distinguishing between minor oozing and excessive bleeding – and meticulously following your post-operative care instructions, you empower yourself to navigate this period with confidence.
Remember, a little bit of pink-tinged saliva is usually nothing to worry about. However, if you experience heavy, persistent bleeding, large blood clots, or any other concerning symptoms like severe pain or fever, do not hesitate to contact your dental professional immediately. They are your primary resource and best guide through the recovery process. Your diligence in both immediate aftercare and long-term maintenance will ensure the longevity and success of your dental implant, providing you with a healthy, beautiful smile for many years to come in 2026 and beyond.
References
[1] American Academy of Periodontology. “Dental Implant Surgery.” Perio.org, 2026.
[2] American Dental Association. “After Dental Implant Placement.” MouthHealthy.org, 2026.
[3] National Institute of Dental and Craniofacial Research. “Dental Implants.” NIDCR.NIH.gov, 2026.
Dental Implant Bleeding Assessment Tool
Use this tool to help assess if your post-operative bleeding after a dental implant procedure is within normal expectations or if you should contact your dentist. Select the option that best describes your situation.

Leave a Reply
Share your thoughts or ask a question about dental implants. Your email address will not be published.