Dental implants are a revolutionary solution for missing teeth, offering a durable and aesthetically pleasing alternative to traditional dentures or bridges. Designed to last for many years, often a lifetime, they are considered a long-term investment in your oral health and confidence. However, just like natural teeth, dental implants are not entirely impervious to issues. Over time, or due to various factors, an implant can develop problems that may necessitate its replacement. Understanding the signs dental implant needs replacement is crucial for prompt intervention, preventing further complications, and ensuring the continued health of your smile. As an expert SEO content strategist and senior editor, I’m here to guide you through the critical indicators that your dental implant might be failing and what steps you should take in 2026.
Key Takeaways
- Persistent Pain or Discomfort: Any ongoing pain, tenderness, or throbbing around the implant site is a significant red flag requiring immediate professional evaluation.
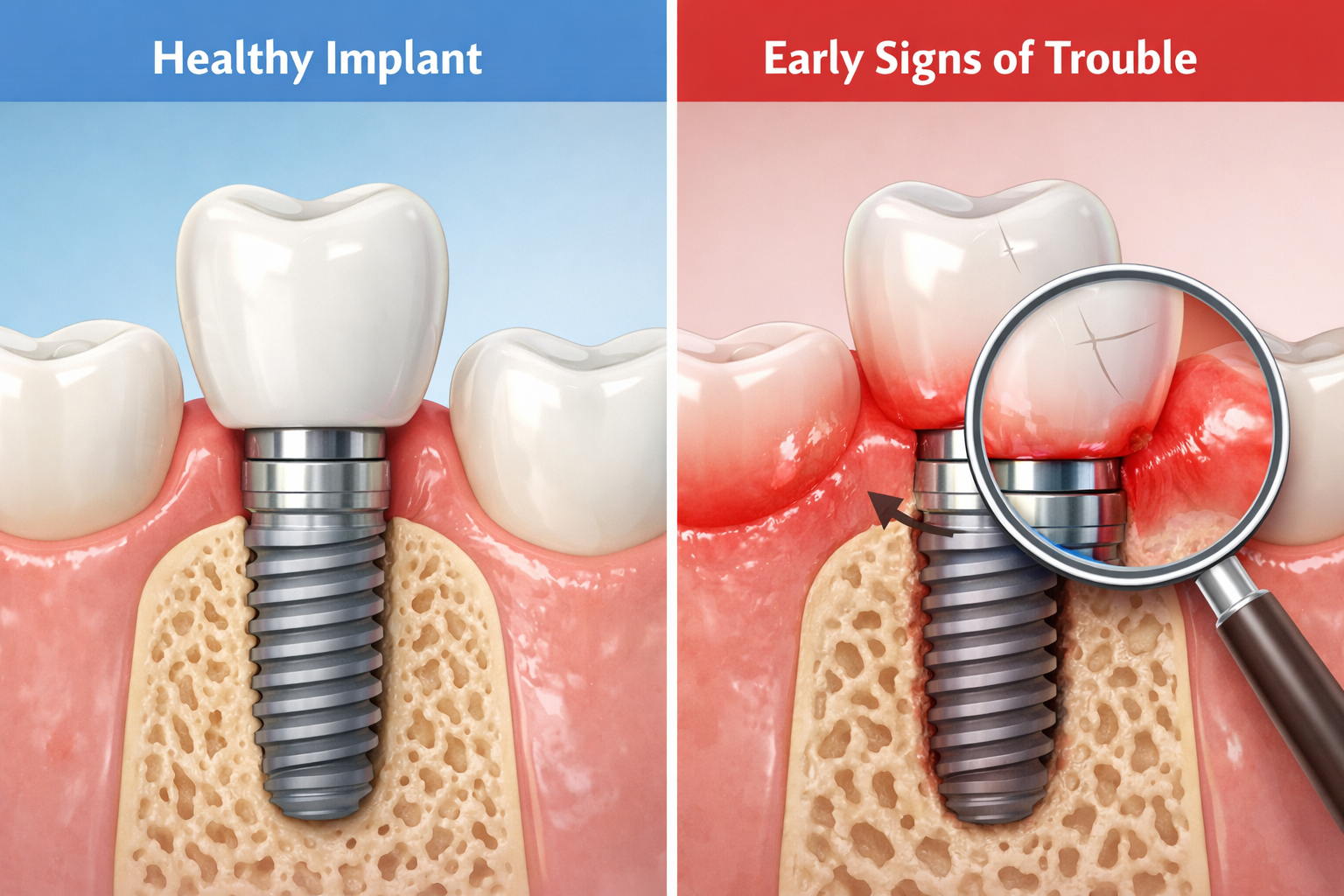
- Visible Loosening or Movement: A dental implant should feel completely stable. Any noticeable movement of the crown, abutment, or the implant post itself indicates a serious problem.
- Gum Inflammation or Infection (Peri-implantitis): Red, swollen, bleeding gums, pus, or a bad taste around the implant are classic signs of peri-implantitis, a common cause of implant failure.
- Difficulty Chewing or Biting: If chewing or biting becomes painful, difficult, or feels unnatural with your implant, it could point to a structural or integration issue.
- Receding Gums or Bone Loss: Exposure of the implant post due to gum recession or significant bone loss around the implant can compromise its stability and necessitate replacement.
Understanding Dental Implant Failure: Why It Happens
While dental implants boast an impressive success rate, typically ranging from 95-98% [1], failures can occur. These failures are generally categorized into two types: early failures and late failures. Early failures happen shortly after placement and are often due to a lack of osseointegration (the process where the implant fuses with the jawbone), infection, or excessive force during healing. Late failures, which are more common and what we’ll focus on when discussing signs dental implant needs replacement, can manifest years after the initial procedure.
Several factors contribute to late implant failure:
- Peri-implantitis: This is arguably the most common cause of late implant failure. Similar to periodontitis (gum disease affecting natural teeth), peri-implantitis is an inflammatory condition affecting the soft tissues and bone surrounding an osseointegrated implant. It’s often caused by bacterial infection and can lead to progressive bone loss and eventual implant mobility.
- Poor Oral Hygiene: Neglecting proper cleaning around your implant can lead to plaque and tartar buildup, fostering bacterial growth and increasing the risk of peri-implantitis.
- Excessive Chewing Forces (Bruxism): Chronic teeth grinding or clenching (bruxism) can place undue stress on the implant and the surrounding bone, potentially leading to fracture, loosening, or bone loss.
- Trauma: Any injury to the mouth or face can directly impact the implant, causing damage to the implant components or the surrounding bone.
- Systemic Health Conditions: Certain medical conditions, such as uncontrolled diabetes, osteoporosis, or autoimmune diseases, can impair bone healing and immune response, increasing the risk of implant failure.
- Smoking: Smoking significantly hinders healing and reduces blood flow, making smokers more susceptible to peri-implantitis and overall implant failure.
- Improper Placement or Poor Bone Quality: While less common in late failures, if the implant was not optimally placed, or if the initial bone quality was insufficient, it can lead to long-term stability issues.
- Component Fracture: Although dental implant materials are robust, components like the crown, abutment, or even the implant post itself can fracture due to extreme forces or material fatigue over many years.
Understanding these underlying causes helps contextualize the signs dental implant needs replacement that we’ll explore in detail.
Recognizing the Early Signs Dental Implant Needs Replacement
Detecting problems early is paramount to successful intervention and potentially saving your existing implant or planning for a replacement with minimal fuss. Pay close attention to these subtle, yet crucial, indicators.
1. Persistent Pain, Discomfort, or Swelling Around the Implant
While some initial discomfort is normal after implant surgery, persistent or worsening pain months or years later is a serious concern. This pain can manifest as a dull ache, throbbing sensation, or sharp pain when chewing. It might be accompanied by swelling or tenderness in the gum tissue surrounding the implant.
“Any pain around a dental implant that lasts more than a few days, or suddenly appears after a period of comfort, warrants immediate attention from your dentist or oral surgeon.”
- What to look for:
- Pain that doesn’t go away after taking over-the-counter pain relievers.
- Pain that intensifies when you apply pressure to the implant (e.g., while chewing).
- Swelling or tenderness in the gums or cheek near the implant site.
- A feeling of constant pressure or throbbing.
Such symptoms often signal an underlying infection (peri-implantitis), nerve damage, or even a hairline fracture in the implant or surrounding bone. Early detection through regular check-ups is vital. Learn more about optimal dental implant care to prevent such issues by visiting our guide on best dental implant aftercare products.
2. Visible Loosening or Movement of the Implant Crown or Abutment
A properly integrated dental implant should feel as stable as a natural tooth. There should be absolutely no movement. If you notice any wobbling, shifting, or a feeling that your implant crown or the abutment (the connector between the implant post and the crown) is loose, it’s a definitive sign of trouble. This can sometimes be confused with a loose crown on a natural tooth, but with an implant, it often indicates a more serious issue.
- How to check:
- Gently try to wiggle the crown with your finger.
- Notice if the crown feels different when you bite down or chew.
- A clicking noise when you chew could also indicate a loose component. For more on this, see our article on dental implant clicking noise.
This loosening could be due to a loose abutment screw, a fractured crown, or, more seriously, a failure of the implant post to remain integrated with the bone. If the implant post itself is loose, it indicates significant bone loss or a failure of osseointegration, meaning the implant post isn’t fused to the bone anymore. This usually means the implant needs replacement.
3. Gum Inflammation, Redness, Bleeding, or Pus Around the Implant (Peri-implantitis)
This is one of the most common and critical signs dental implant needs replacement. Peri-implantitis is an inflammatory condition that can progress to affect the bone supporting the implant. It’s often painless in its early stages, making regular dental check-ups and good oral hygiene paramount.
- Symptoms of peri-implantitis:
- Red, swollen gums around the implant, appearing much darker than healthy gum tissue.
- Bleeding gums when brushing, flossing, or even spontaneously.
- Tenderness or pain in the gum tissue.
- Pus discharge from around the implant, which might also cause a persistent bad taste or bad breath.
- Receding gums, revealing part of the metal implant or abutment.
- Deepening gum pockets around the implant (measured by your dentist).
If left untreated, peri-implantitis can lead to significant bone loss, weakening the implant’s support and eventually leading to its failure. This condition is a primary driver for the need for replacement.
4. Difficulty Chewing or Biting with the Implant
If your dental implant functioned perfectly for years but now causes pain or discomfort when you chew or bite, or if it feels “off,” it’s a sign that something is amiss. This could range from minor issues like an ill-fitting crown to more severe problems such as bone loss around the implant.
- Indications:
- Pain when biting down on specific foods.
- A feeling that the implant crown is hitting other teeth incorrectly.
- Avoiding chewing on the side of the mouth with the implant.
- Persistent dull ache after meals.
This difficulty can also be a symptom of a fractured crown or abutment, or even a microfracture in the jawbone surrounding the implant, all of which point towards potential replacement.
Advanced Signs Dental Implant Needs Replacement
While the early signs are crucial for timely intervention, some issues represent a more advanced stage of implant failure, making replacement almost inevitable.
5. Significant Gum Recession or Exposure of the Implant Post
Over time, or due to peri-implantitis, aggressive brushing, or even the initial placement, the gum tissue around an implant can recede. If you notice the metal implant post or the abutment becoming visible above the gum line, it’s a significant indicator of an issue.
- What to observe:
- A noticeably longer-looking implant crown compared to adjacent teeth.
- Seeing the grey or metallic part of the implant that should be covered by gum tissue.
- Increased sensitivity in the area.
Gum recession often indicates bone loss underneath, as the gum tissue tends to follow the bone level. When the implant body is exposed, it becomes harder to clean, further exacerbating the risk of infection and accelerating bone loss. In some cases, severe gum recession can be an advanced sign dental implant needs replacement.
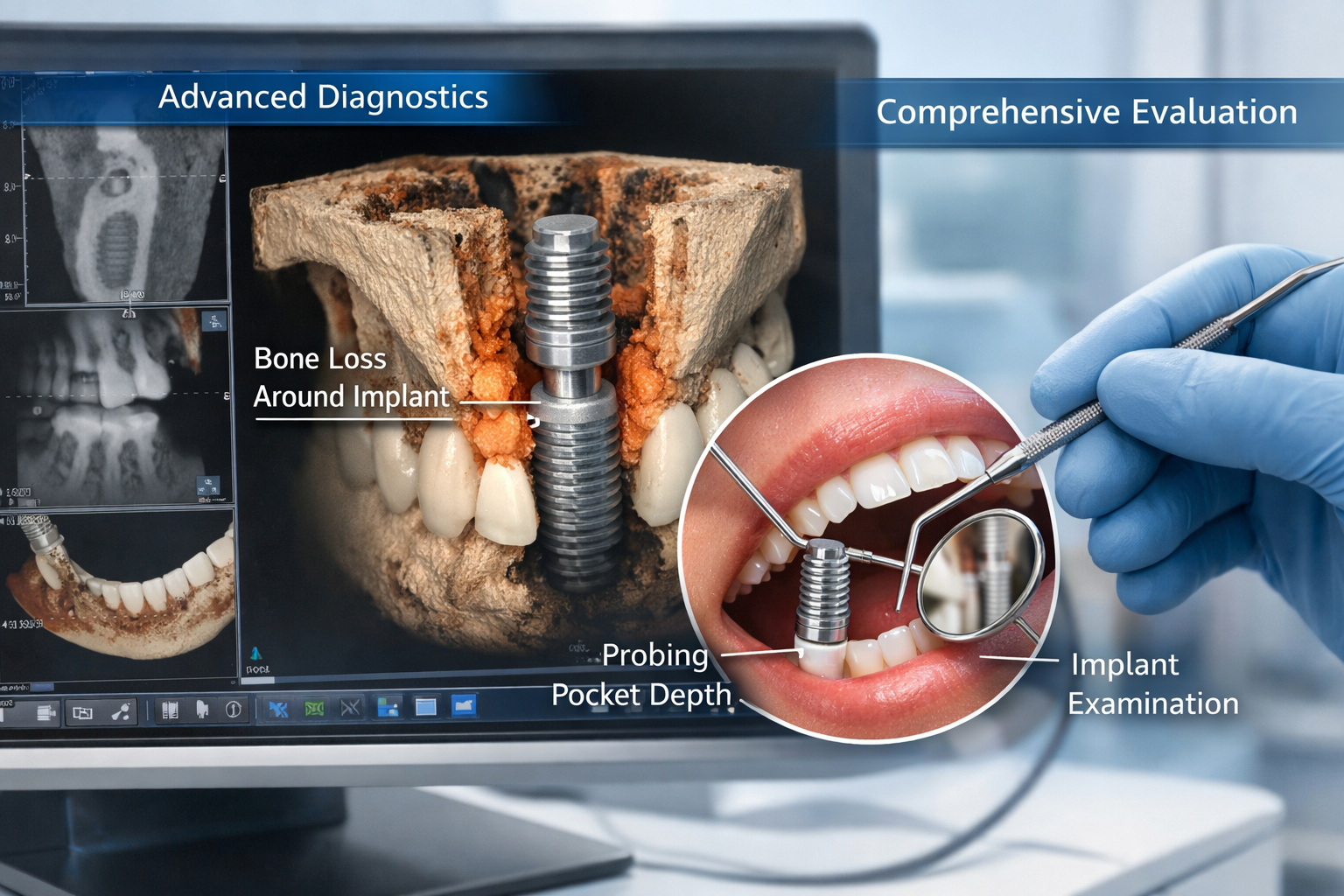
6. Noticeable Bone Loss Around the Implant (Diagnosed by X-ray)
Bone loss around an implant is a serious concern, as the implant’s stability relies entirely on its integration with the jawbone. While minor bone remodeling can occur after implant placement, significant progressive bone loss is abnormal and usually indicates a failing implant. This is typically diagnosed through dental X-rays or 3D CT scans performed by your dentist.
- What it means:
- The implant is losing its foundational support.
- Often a direct result of untreated peri-implantitis.
- Can lead to implant mobility and eventual complete failure.
If your dentist shows you X-rays indicating significant bone loss around an implant, especially if it’s accompanied by other symptoms, it’s a strong indicator that the implant is failing and likely needs replacement. In cases of severe bone loss, a bone graft may be necessary before a new implant can be placed. Learn more about bone grafts for dental implants.
7. Changes in Bite or Alignment of Adjacent Teeth
If a dental implant is failing, the instability can subtly impact the surrounding teeth and your overall bite. While this is less common than other signs, it’s worth noting.
- Possible observations:
- Your teeth don’t fit together as they used to.
- New gaps appearing between teeth.
- Discomfort or pain in other teeth, possibly due to shifting forces.
These changes are usually secondary to the implant’s instability or bone loss, highlighting the interconnectedness of your oral health.
8. Fractured Implant Components
Though rare, the implant post itself or the abutment can fracture. This typically occurs due to excessive force over time, chronic bruxism, or trauma.
- Indicators:
- Sudden, severe pain.
- Acute loosening of the crown.
- An inability to chew on the affected side.
- A visible crack in the crown or abutment (sometimes only detectable by a dentist).
A fractured implant post almost always necessitates removal and replacement. If it’s just the crown or abutment, those components might be replaced without removing the implant, but a dental professional needs to make that determination. For more details on abutment placement and related components, you can read our guide on the complete guide to the dental implant abutment procedure.
When to See a Dentist in 2026
The moment you notice any of these signs dental implant needs replacement, it’s critical to schedule an appointment with your dentist or oral surgeon without delay. Early diagnosis and intervention can often prevent the problem from worsening and might even save your implant. Waiting too long can lead to more extensive damage, more complex treatment, and higher costs.
During your visit, the dentist will:
- Conduct a thorough oral examination: Visually inspecting the implant, surrounding gums, and adjacent teeth.
- Probe the gum pockets: To check for inflammation and measure pocket depth, which can indicate peri-implantitis and bone loss.
- Take X-rays or 3D CT scans: To assess the bone level around the implant, check for fractures, and evaluate the overall health of the jawbone.
- Test for mobility: Gently checking if the implant crown, abutment, or the implant itself is loose.
Based on these findings, your dentist will determine the cause of the problem and recommend the most appropriate course of action. This could range from non-surgical treatments like antibiotics and professional cleanings for early peri-implantitis, to surgical interventions like guided bone regeneration, or, in more severe cases, removal of the failing implant and eventual replacement.
The Process of Dental Implant Replacement
If your dentist confirms that your dental implant needs replacement, the process will generally involve several steps:
- Removal of the Failing Implant: The existing implant post will be carefully removed. This can sometimes be done non-surgically if the implant is very loose, but often requires a minor surgical procedure.
- Addressing the Underlying Issue: If bone loss or infection was the cause, these issues must be addressed. This might involve thorough cleaning of the area, antibiotics, and often a bone grafting procedure to rebuild the jawbone foundation. You can find more information about dental bone graft healing here.
- Healing Period: The site needs time to heal after the implant removal and any bone grafting. This healing period can vary significantly, from a few weeks to several months, depending on the extent of bone regeneration needed.
- New Implant Placement: Once the area has fully healed and sufficient bone density is present, a new dental implant can be surgically placed.
- Osseointegration: The new implant will then need several months to fuse with the jawbone.
- Abutment and Crown Placement: After successful osseointegration, an abutment is attached, followed by a custom-made crown, restoring your tooth’s function and appearance.
The journey to replace a failing implant can be extensive, underscoring the importance of vigilance and prompt dental care if you suspect any of the signs dental implant needs replacement. For comprehensive information on dental implants and their care, feel free to explore our main page at https://dentalimplantsdallastx.com/.
Maintaining Your Dental Implants for Long-Term Success
While knowing the signs of failure is crucial, prevention is always better than cure. Here’s how you can maximize the lifespan of your dental implants and minimize the chances of needing a replacement in 2026 and beyond:
- Practice Excellent Oral Hygiene: Brush twice a day with a soft-bristled toothbrush, floss daily (or use specialized interdental brushes/water flossers for implants), and use an antimicrobial mouthwash if recommended by your dentist.
- Regular Dental Check-ups and Professional Cleanings: Visit your dentist every six months, or more frequently if advised, for professional cleanings and examinations. Your dental hygienist has specialized tools to clean around implants without causing damage.
- Avoid Hard and Sticky Foods: While implants are strong, excessively hard foods (like nuts, hard candies) or sticky foods can put undue stress on the crown and underlying implant components.
- Manage Bruxism: If you grind or clench your teeth, especially at night, talk to your dentist about a custom-made night guard. This protective appliance can significantly reduce the forces on your implants and natural teeth.
- Quit Smoking: Smoking is a major risk factor for implant failure. Quitting can dramatically improve your implant’s longevity and overall oral health.
- Address Systemic Health Issues: Keep any underlying medical conditions, such as diabetes, well-managed. Inform your dentist about any health changes or medications you are taking.
By diligently following these guidelines, you significantly reduce the likelihood of encountering the signs dental implant needs replacement.
Conclusion
Dental implants offer a fantastic, long-lasting solution for tooth loss, providing stability, function, and aesthetics that can last decades. However, they are not immune to problems, and recognizing the signs dental implant needs replacement is key to preserving your oral health and investment. From persistent pain and visible loosening to gum inflammation and bone loss, vigilance and prompt action are your best allies.
If you observe any of the symptoms discussed in this article, do not hesitate. Contact your dental professional immediately. Early diagnosis by an experienced dentist or oral surgeon in 2026 can lead to timely intervention, potentially preventing further complications, and guiding you towards the most effective solution, whether that’s treatment to save your current implant or a plan for a successful replacement. Your proactive approach is the best way to ensure your smile remains healthy, functional, and beautiful for years to come.
References
[1] Alsaeed, A. O., et al. (2018). “Success and Survival Rate of Dental Implants: A Systematic Review.” Journal of Clinical and Diagnostic Research, 12(10), ZE01–ZE05.
Dental Implant Health Self-Assessment (2026)
This tool helps you quickly assess if you might be experiencing signs dental implant needs replacement. Answer truthfully based on your recent experiences.
Your Implant Health Assessment:
Remember, this is a self-assessment. Only a dental professional can provide an accurate diagnosis.
This tool is for informational purposes only and does not constitute medical advice. Always consult with a qualified dental professional for any concerns regarding your dental implants.


Leave a Reply
Share your thoughts or ask a question about dental implants. Your email address will not be published.