The journey to restoring a full, confident smile often culminates in dental implant placement, a sophisticated and highly effective solution for missing teeth. However, for individuals who experience bruxism – the involuntary clenching or grinding of teeth – the success and longevity of these remarkable prosthetics can be significantly jeopardized. Understanding the nuances of teeth grinding dental implant damage is paramount for both patients and practitioners in 2026, enabling proactive measures and informed treatment decisions. This article will delve deep into how bruxism impacts dental implants, the signs to watch for, and the most effective strategies for prevention and management, ensuring your investment in oral health endures for years to come.
Key Takeaways
- Bruxism Poses a Significant Threat: Teeth grinding and clenching apply excessive, non-axial forces to dental implants, leading to potential complications such as crown fracture, abutment loosening, bone loss, and even implant failure.
- Early Detection is Crucial: Recognizing symptoms like jaw pain, headaches, clicking noises, or visible wear on natural teeth and implant crowns allows for timely intervention to prevent severe damage.
- Custom Night Guards are Essential: A professionally fitted occlusal splint or night guard is often the first line of defense, distributing forces evenly and protecting implants from direct impact during sleep.
- Comprehensive Management is Multifaceted: Effective treatment involves addressing underlying causes of bruxism (stress, sleep disorders), occlusal adjustments, and, in some cases, advanced therapies like Botox to reduce muscle activity.
- Regular Dental Check-ups are Non-Negotiable: Routine visits enable dentists to monitor implant health, assess for signs of bruxism-related stress, and perform necessary adjustments or interventions to preserve implant longevity.
Understanding the Mechanics of Teeth Grinding and its Impact on Dental Implants
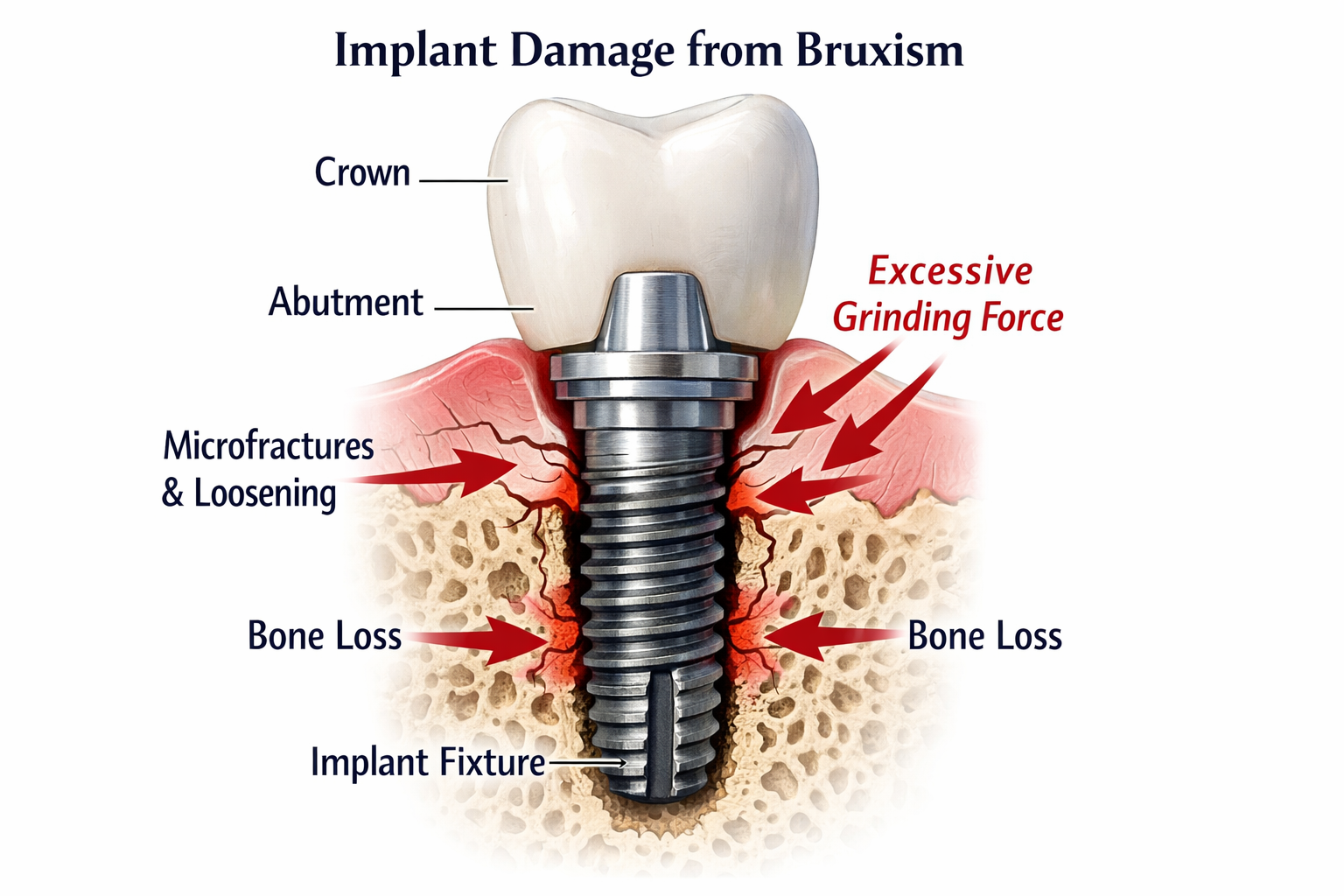
Teeth grinding, medically known as bruxism, is a common condition that affects many people, often subconsciously during sleep (sleep bruxism) or while awake (awake bruxism) [1]. This habitual clenching, grinding, or gnashing of teeth generates significant forces – sometimes hundreds of pounds per square inch – that far exceed those experienced during normal chewing. While natural teeth possess a periodontal ligament that provides some shock absorption, dental implants are rigidly anchored to the jawbone through a process called osseointegration [2]. This direct, inflexible connection means that the excessive forces from bruxism are transmitted almost entirely to the implant components and the surrounding bone, increasing the risk of teeth grinding dental implant damage.
The Unique Vulnerability of Dental Implants
Unlike natural teeth, which have a built-in shock-absorbing mechanism (the periodontal ligament), dental implants are fused directly to the bone. This offers exceptional stability but also means they lack the natural give that helps dissipate occlusal forces. When someone with bruxism has dental implants, these constant, heavy forces can lead to several problems:
- Mechanical Stress: The repeated, often sideways, forces can stress the implant crown, the abutment (the connector between the implant and the crown), and the implant fixture itself. This can lead to wear, chipping, or fracturing of the crown, loosening of the abutment screw, or even fracture of the implant [3].
- Bone Overload: The bone surrounding the implant, while strong, can be subjected to excessive stress. This can impede the healing process for newer implants or, in established implants, lead to peri-implant bone loss, a condition similar to periodontal disease but affecting implants [4]. Over time, this bone loss can compromise the implant’s stability.
- Lack of Proprioception: Natural teeth have sensory nerves that tell the brain how much force is being applied during chewing, allowing for fine-tuned control. Implants lack these nerves, meaning a bruxer may not perceive the destructive forces they are exerting until damage has already occurred.
The critical difference lies in the biomechanical response. Natural teeth can shift slightly under pressure, distributing forces across a broader area. Implants, being rigid, concentrate these forces at the bone-implant interface and within the prosthetic components, making them more susceptible to failure when subjected to the extreme loads of bruxism.
Recognizing the Signs of Teeth Grinding Dental Implant Damage
Detecting teeth grinding dental implant damage early is paramount to preventing more severe complications and ensuring the longevity of your dental investment. The signs can be subtle at first but become more pronounced as the problem progresses. Patients and their dental care providers must be vigilant in identifying these indicators.
Common Symptoms and What They Mean
| Symptom Category | Specific Signs | What It Indicates |
|---|---|---|
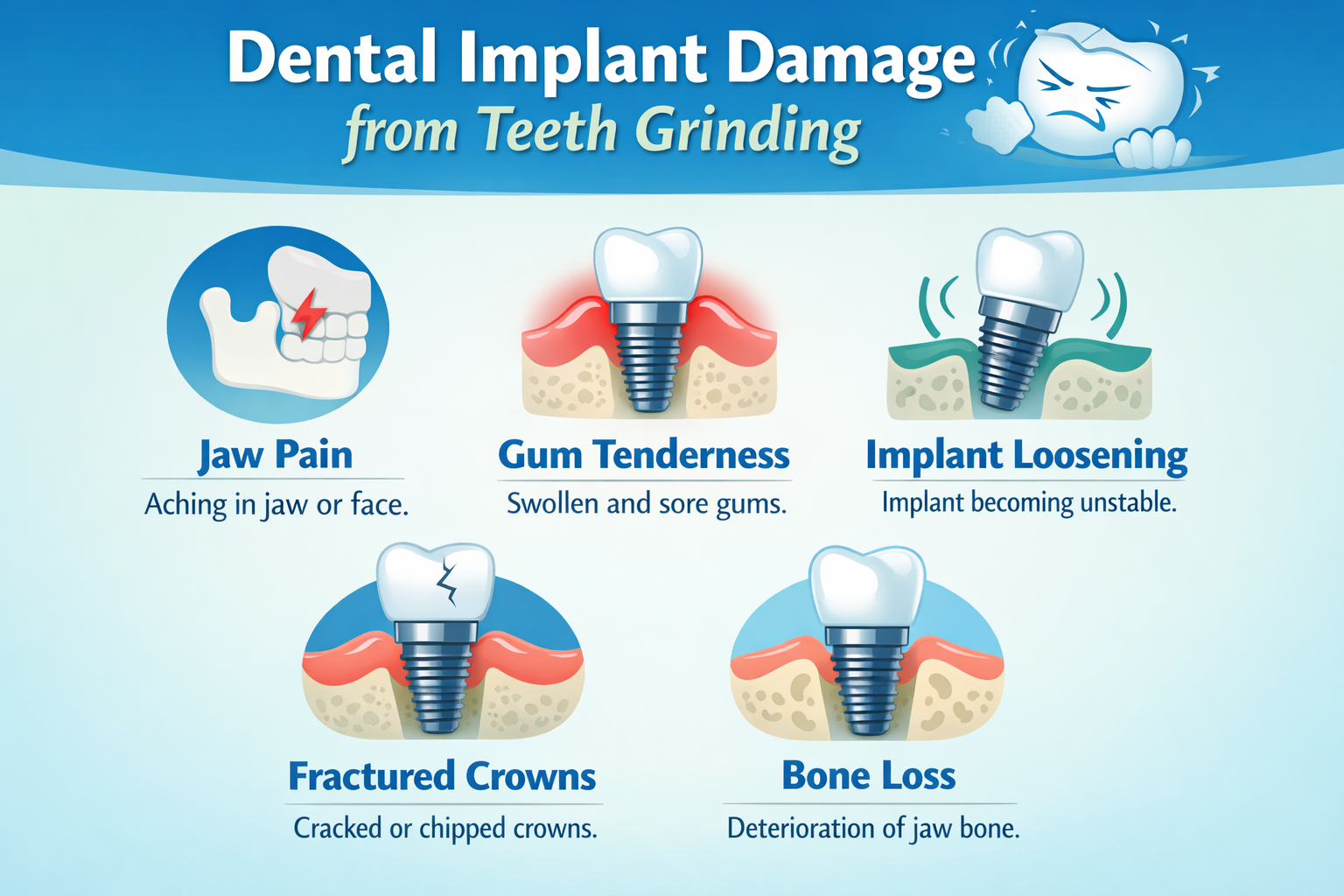
| Oral Pain/Discomfort | Generalized jaw pain, facial muscle soreness, headaches (especially in the temples or upon waking), earaches, sensitivity in implants or surrounding teeth. | These are classic signs of overworked jaw muscles and temporomandibular joint (TMJ) stress caused by constant clenching and grinding. Pain directly around the implant could signal inflammation or excessive pressure on the surrounding bone. |
| Prosthetic Damage | Chipped, cracked, or fractured implant crowns; loose crowns; visible wear facets on the implant crown (flat, polished areas); recurrent loosening of abutment screws. | Direct evidence of the mechanical stress from bruxism. Crowns are designed to withstand normal chewing forces, but grinding generates much higher, often shearing, forces. A loose crown or abutment indicates that the connection is failing under stress, requiring prompt attention to avoid further damage to the implant itself. |
| Implant Mobility | The implant crown feels loose or wobbly; clicking or unusual sounds when chewing or moving the jaw. | A healthy dental implant should be completely stable. Any noticeable movement or clicking sound is a serious red flag. It could indicate a loose abutment screw, a fractured implant component, or, most critically, a failure of the osseointegration process, leading to implant failure. Immediate dental consultation is essential if you experience this. Learn more about dental implant clicking noises. |
| Gum & Bone Changes | Gum recession around the implant; redness or inflammation of the gum tissue; bone loss visible on X-rays. | While gum inflammation can be due to poor hygiene (peri-implantitis), excessive occlusal forces can exacerbate it or directly contribute to peri-implant bone loss. The constant pressure can lead to the breakdown of the bone supporting the implant, which is a critical aspect of teeth grinding dental implant damage. Your dentist will typically identify bone loss through diagnostic imaging. |
| Sleep Disturbances | Waking up with a sore jaw or headache; reports from a partner of grinding noises during sleep. | These are direct indications of sleep bruxism, which is a significant risk factor for implant damage. Many individuals are unaware they grind their teeth during sleep until a partner informs them or they experience related symptoms. |
If any of these signs are noticed, it is crucial to schedule an appointment with a dental professional experienced in implant dentistry without delay. Early intervention can often prevent irreversible damage and save the implant.
The Progression of Damage: From Microfractures to Implant Failure
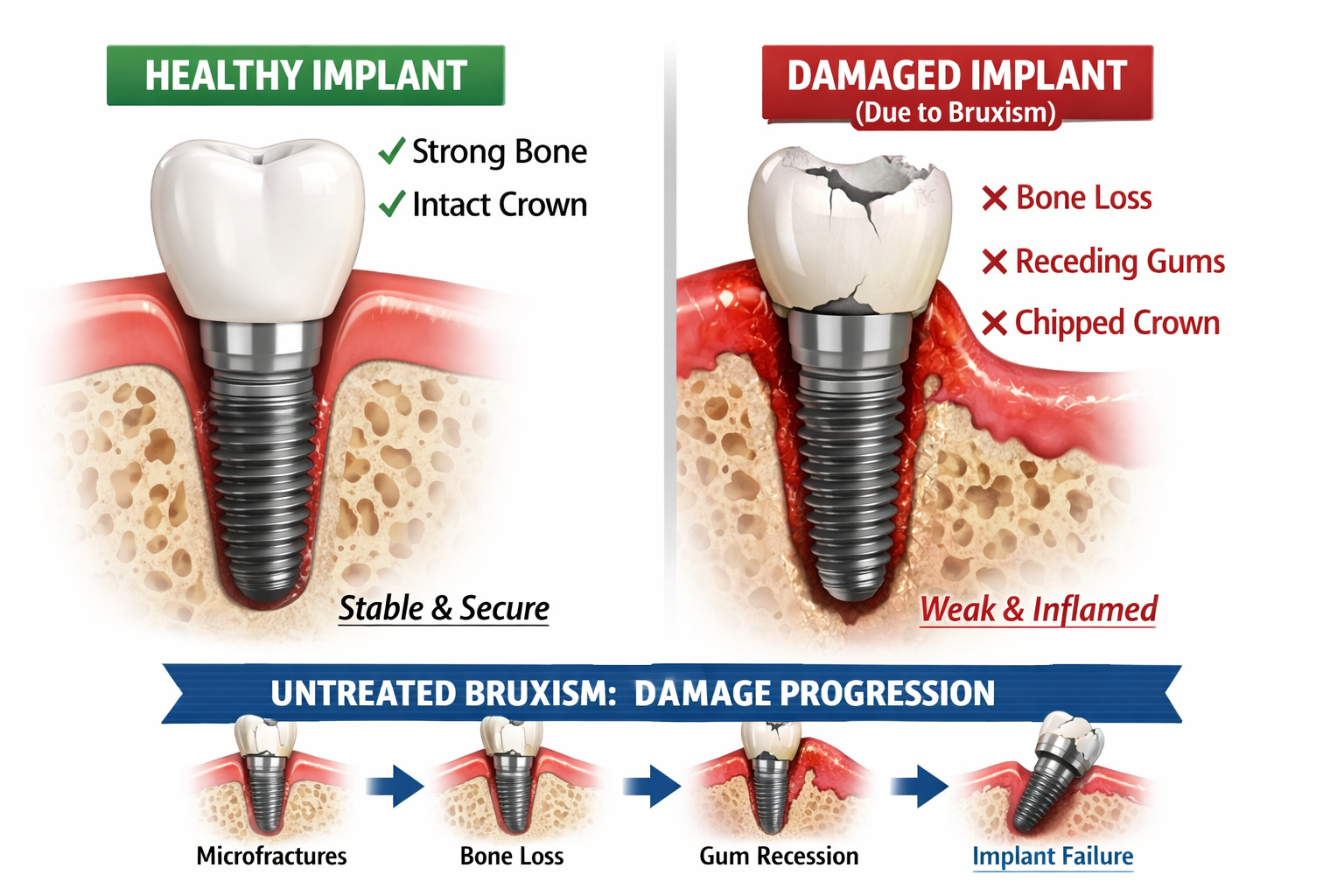
The effects of unmanaged bruxism on dental implants are not immediate but rather a progressive process, much like continuous stress on any complex structure. Understanding this progression can underscore the importance of early intervention when dealing with teeth grinding dental implant damage.
Stages of Damage
Initial Stress & Microtrauma:
- Crown Wear and Chipping: The first noticeable signs often appear on the implant crown. The constant friction and pressure can lead to accelerated wear, developing flattened surfaces (facets), or small chips and fractures in the porcelain or composite material.
- Abutment Screw Loosening: The abutment, which connects the crown to the implant, is typically secured with a small screw. Excessive lateral forces can cause this screw to gradually loosen, leading to a feeling of slight movement or a “clicking” sound. This is a common early indicator.
- Gum Inflammation: While peri-implantitis is primarily bacterial, constant trauma from bruxism can irritate the gum tissue around the implant, making it more susceptible to inflammation and recession.
Developing Complications:
- Bone Stress and Resorption: The rigid nature of the implant means forces are directly transferred to the surrounding bone. Prolonged, excessive loading can lead to what is known as “overload,” causing microfractures in the bone. The body’s response to this chronic trauma is often to resorb (lose) the bone around the implant, particularly the crestal bone (the bone at the top of the implant). This bone loss reduces the implant’s stability.
- Abutment Fracture/Implant Component Failure: If the abutment screw repeatedly loosens or if the forces are extreme, the abutment itself can fracture. In rare but severe cases, the implant fixture (the part embedded in the bone) can fracture, especially in areas of bone loss or if the implant material has been weakened.
Advanced Damage & Implant Failure:
- Progressive Implant Mobility: As bone loss advances or components fail, the implant will become noticeably mobile. This is a critical stage, indicating a significant compromise to the implant’s structural integrity.
- Infection and Further Bone Loss: A failing implant with compromised seals or mobility can become a site for bacterial colonization, leading to peri-implantitis, an infection that further accelerates bone loss and compromises the implant.
- Complete Implant Failure: Ultimately, if the damage progresses unchecked, the implant may completely fail, requiring its removal. This necessitates further surgical procedures, potentially including bone grafting (for more information, see bone grafts for dental implants), before another implant can be placed, if at all possible.
Pull Quote: “Unmanaged bruxism can transform a successful dental implant into a ticking time bomb. Early detection and proactive intervention are not just recommended, they are absolutely critical to safeguarding your smile.”
The cumulative effect of these stresses means that what starts as a minor chip can eventually lead to the complete loss of a dental implant. This highlights the importance of regular dental check-ups, especially for patients with a history of bruxism, to identify and address these issues before they escalate.
Strategies for Preventing and Managing Teeth Grinding Dental Implant Damage
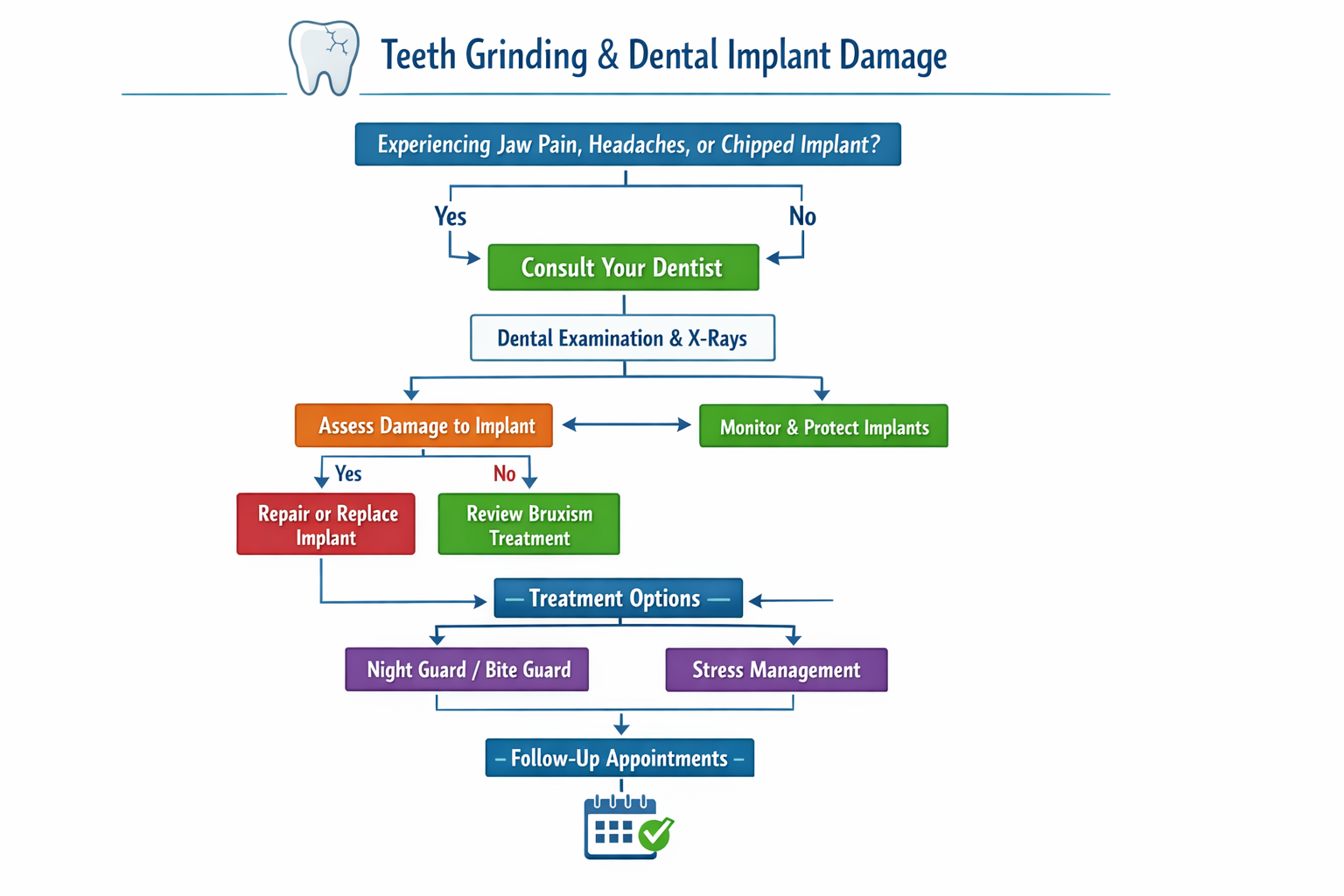
Preventing and managing teeth grinding dental implant damage requires a multi-faceted approach. Because bruxism often has several contributing factors, an effective strategy typically combines dental interventions with lifestyle modifications.
1. Custom Occlusal Splints (Night Guards)
This is often the first and most crucial line of defense.
- How they work: A custom-made occlusal splint, often called a night guard, is a removable appliance made of durable acrylic that fits precisely over the upper or lower teeth. It creates a physical barrier between the upper and lower arches, preventing direct tooth-on-tooth contact and distributing the grinding forces more evenly across the entire arch.
- Benefits for implants: For dental implant patients, a night guard protects the implant crown from wear and fracture, reduces stress on the abutment and implant fixture, and helps mitigate the forces transmitted to the surrounding bone. It also helps relax the jaw muscles, reducing overall clenching intensity.
- Importance of Custom Fit: Over-the-counter boil-and-bite guards are generally not recommended for bruxism, especially for implant patients. A custom-fabricated guard from a dentist ensures optimal fit, comfort, and proper occlusal (bite) balance, which is vital for protecting implants.
2. Occlusal Adjustments
- Balancing the Bite: Sometimes, an uneven bite (occlusion) can contribute to bruxism or direct excessive force to specific teeth or implants. Your dentist may perform minor adjustments to the chewing surfaces of your implant crowns or natural teeth to create a more harmonious bite. This ensures that forces are distributed evenly, reducing localized stress points.
- Post-Implant Care: After implant placement and crown delivery, careful assessment of the bite is always performed. However, changes can occur over time, or subtle imbalances might only become apparent under the intense forces of bruxism. Regular follow-up appointments, such as those recommended for dental implant aftercare, are important for ongoing evaluation.
3. Addressing the Root Causes of Bruxism
Bruxism is often linked to underlying factors, which, if addressed, can significantly reduce grinding activity.
- Stress and Anxiety Management: Stress is a primary trigger for bruxism. Techniques like meditation, yoga, cognitive behavioral therapy (CBT), or counseling can help manage stress levels.
- Sleep Disorder Treatment: Sleep bruxism is frequently associated with sleep disorders like sleep apnea. If suspected, a sleep study may be recommended. Treating sleep apnea can often reduce or eliminate sleep bruxism.
- Medication Review: Certain medications, such as some antidepressants, can have bruxism as a side effect. Discussing your medications with your doctor can help identify potential culprits.
- Lifestyle Changes: Reducing caffeine and alcohol intake, especially before bed, can sometimes lessen bruxism severity. Quitting smoking may also help, as nicotine is a stimulant.
4. Advanced Therapies
For severe or persistent cases, your dentist might recommend more advanced interventions:
- Botox Injections: Small injections of botulinum toxin (Botox) into the masseter muscles (jaw muscles) can temporarily weaken them, reducing the intensity of clenching and grinding. This can provide significant relief and reduce forces on implants, lasting for several months before needing re-treatment.
- Biofeedback: This technique involves using electronic devices to monitor jaw muscle activity. Patients learn to recognize when they are clenching and develop strategies to relax their jaw muscles.
- Physical Therapy: For patients with significant jaw pain or TMJ dysfunction related to bruxism, physical therapy may be beneficial.
5. Regular Dental Monitoring
Even with preventive measures, continuous monitoring by your dental team is vital.
- Routine Check-ups: During your regular check-ups (typically every 6 months to a year), your dentist will thoroughly examine your implants and surrounding tissues, assess for signs of wear on your night guard, and check for any new signs of bruxism or implant stress. This is crucial for early detection and intervention.
- X-rays: Periodic X-rays allow your dentist to monitor the bone levels around your implants and detect any changes indicative of bone loss due to excessive force.
By combining these strategies, patients with dental implants who grind their teeth can significantly reduce their risk of teeth grinding dental implant damage and ensure the long-term success and health of their new smile. It is a collaborative effort between the patient and the dental care team.
The Role of Dental Professionals in Mitigating Damage

The expertise and vigilance of dental professionals are indispensable in preventing and managing teeth grinding dental implant damage. From the initial treatment planning to long-term maintenance, their role is central to safeguarding the patient’s oral health investment.
Comprehensive Assessment and Planning
- Pre-Implant Evaluation: Before any implant placement, a thorough assessment of the patient’s oral health and medical history is conducted. This includes identifying any history or signs of bruxism. If bruxism is suspected or confirmed, it significantly influences the treatment plan.
- Implant Selection and Placement: For bruxers, dentists may opt for:
- Wider and/or longer implants: To provide a larger surface area for osseointegration and better distribute forces [5].
- Implants placed in a more favorable bone density: To enhance stability.
- Careful consideration of implant angulation: To ensure optimal load distribution and minimize lateral forces.
- Material choice: Stronger, more durable materials for crowns and abutments might be chosen to withstand higher forces.
- Occlusal Design: The dental team meticulously designs the occlusal surfaces of the implant crowns. This involves creating a bite that minimizes heavy contacts and distributes chewing forces evenly, especially during excursive (side-to-side) movements, which are common during grinding. This is particularly important for complex restorations like all-on-4 dental implants or full-mouth rehabilitation.
Post-Placement Monitoring and Intervention
- Immediate Post-Op Instructions: Patients are educated on the importance of avoiding clenching and grinding during the initial healing phase. Instructions for soft foods after dental implant surgery are also crucial to minimize force on the new implants.
- Regular Follow-Up Appointments: As mentioned, routine check-ups are essential. During these visits, dentists will:
- Visually inspect the implant crowns for wear, chips, or fractures.
- Check for any signs of abutment screw loosening or implant mobility.
- Palpate jaw muscles for tenderness or hypertrophy (enlargement) indicative of clenching.
- Take periodic X-rays to monitor bone levels around the implants and detect any bone loss.
- Evaluate the patient’s night guard for wear and fit, replacing it if necessary.
- Proactive Adjustments: If signs of bruxism-related stress are observed, the dentist can make timely adjustments to the bite, recommend a new night guard, or explore other therapeutic options. Early intervention can often prevent irreversible teeth grinding dental implant damage.
Patient Education and Collaboration
- Raising Awareness: Dentists play a vital role in educating patients about the risks of bruxism to dental implants and the importance of adherence to preventive measures. Many patients are unaware of their grinding habits or the potential consequences.
- Personalized Action Plans: Based on the individual patient’s needs, a personalized management plan is developed. This might include recommendations for stress management, sleep specialist referrals, or other adjunct therapies.
- Open Communication: Encouraging patients to report any symptoms, discomfort, or changes in their bite is critical for ongoing care. The relationship between patient and dentist is a partnership in maintaining implant health.
By integrating these professional practices, dental teams can significantly enhance the long-term prognosis of dental implants, even in patients prone to bruxism. This dedicated approach ensures that the functional and aesthetic benefits of dental implants are sustained for many years.
Long-Term Prognosis and What to Expect in 2026
The longevity of dental implants, often touted as a lifelong solution, is indeed remarkable. However, this promising prognosis is heavily reliant on effective management of risk factors, particularly bruxism. For patients with dental implants in 2026, understanding the long-term outlook with and without proper management of teeth grinding is crucial.
Prognosis with Effective Bruxism Management
When bruxism is effectively managed, the long-term prognosis for dental implants is excellent.
- Normal Lifespan: With a custom night guard, regular dental check-ups, and addressing underlying causes, dental implants can comfortably last for decades, often a lifetime.
- Reduced Complications: The risk of mechanical complications (crown fracture, abutment loosening) and biological complications (bone loss, peri-implantitis) is significantly reduced.
- Maintained Oral Health: Patients can continue to enjoy the full benefits of their implants: stable chewing function, preserved jawbone, and a confident smile, without the constant worry of damage.
- Cost-Effectiveness: Proactive management, while requiring an initial investment in a night guard and consistent follow-up, is far more cost-effective than repeatedly repairing or replacing damaged implants. The average cost of dental implants can vary, and preventing damage saves significant expenses over time (for more on costs, see affordable dental implants Dallas TX).
Prognosis Without Effective Bruxism Management
Conversely, if bruxism is left unmanaged or poorly controlled, the long-term outlook for dental implants can be significantly compromised.
- Accelerated Wear and Tear: Expect frequent chipping, cracking, or fracturing of implant crowns. This means repeated dental visits for repairs or replacements, which can be costly and inconvenient.
- Increased Risk of Abutment and Implant Fracture: The persistent, excessive forces increase the likelihood of abutment screw loosening, abutment fracture, and in severe cases, fracture of the implant fixture itself. Implant fracture often necessitates implant removal and potentially complex bone grafting procedures before re-implantation.
- Progressive Bone Loss: Uncontrolled bruxism can lead to chronic microtrauma and accelerated bone resorption around the implants. This peri-implant bone loss can destabilize the implant, eventually leading to its mobility and failure.
- Implant Failure: Ultimately, untreated teeth grinding dental implant damage can lead to complete implant failure, requiring the removal of the implant. This can be a disheartening outcome for patients who have invested significantly in their oral health.
- Compromised Quality of Life: Persistent pain, discomfort, and the need for continuous repairs can severely impact a patient’s quality of life, affecting their ability to chew comfortably and speak clearly, and causing ongoing stress and anxiety.
Evolving Solutions in 2026
The field of implant dentistry continues to advance in 2026. Researchers are exploring new materials for crowns and abutments that offer greater resistance to bruxism-related forces, as well as innovations in implant design that better dissipate stress. Digital dentistry allows for even more precise occlusal analysis and custom night guard fabrication. These advancements, coupled with a proactive approach to bruxism management, are paving the way for even more durable and successful implant outcomes in the future.
The key message remains: dental implants are an exceptional long-term solution, but their longevity in a bruxing patient is a direct reflection of how diligently the condition is managed. Collaboration with your dental team and adherence to recommended therapies are paramount to protecting your investment and maintaining a healthy, functional smile.
Conclusion
Dental implants represent a pinnacle of modern restorative dentistry, offering unparalleled stability, function, and aesthetics for missing teeth. However, the presence of bruxism – the powerful, often unconscious act of teeth grinding and clenching – introduces a significant challenge to their long-term success. The potential for teeth grinding dental implant damage is a serious consideration that demands vigilance and a proactive approach.
From the insidious microtrauma that can lead to chipped crowns and loose abutments, to the more severe complications of peri-implant bone loss and eventual implant failure, the destructive forces of bruxism cannot be underestimated. Recognizing the early warning signs, such as jaw pain, headaches, or even subtle changes in how your implant feels, is the first critical step toward prevention.
In 2026, the good news is that with dedicated care and a collaborative effort between patient and dental professional, this damage is largely preventable and manageable. Custom-fitted occlusal splints (night guards) serve as an indispensable barrier, while careful occlusal adjustments ensure balanced forces. Addressing the underlying causes of bruxism, whether through stress management, treatment of sleep disorders, or advanced therapies like Botox, offers a holistic path to protection.
Actionable Next Steps
If you have dental implants or are considering them, and you suspect you grind or clench your teeth, take these immediate steps:
- Schedule a Consultation: Contact your dental professional experienced in implant dentistry without delay. Discuss any symptoms you’re experiencing or your history of bruxism. You can find experienced professionals at dental implants Dallas TX.
- Discuss a Custom Night Guard: Inquire about getting a professionally fabricated occlusal splint. This is often the most effective initial intervention.
- Be Observant: Pay attention to any jaw pain, headaches, or changes in your implant crowns. Report these promptly to your dentist.
- Explore Underlying Causes: Work with your dentist and, if necessary, other healthcare providers, to identify and address any contributing factors to your bruxism, such as stress or sleep disorders.
- Commit to Regular Check-ups: Adhere to your dentist’s recommended schedule for follow-up appointments and professional cleanings. These visits are vital for monitoring implant health and detecting issues early.
By taking these proactive measures, you can significantly enhance the longevity of your dental implants and continue to enjoy the full benefits of a healthy, functional, and beautiful smile for many years to come. Your investment in dental implants is an investment in your quality of life – protect it diligently.
References
[1] Lobbezoo, F., Ahlberg, J., Glaros, G. R., Kato, T., Koyano, M., Lavigne, G. J., … & Svensson, P. (2013). Bruxism defined and graded: an international consensus. Journal of Oral Rehabilitation, 40(1), 2-4.
[2] Brånemark, P. I., Zarb, G. A., & Albrektsson, T. (1985). Tissue-Integrated Prostheses: Osseointegration in Clinical Dentistry. Quintessence Publishing Co.
[3] Misch, C. E. (2015). Dental Implant Prosthetics. Elsevier Mosby.
[4] Renvert, S., & Polyzois, I. (2018). Clinical advances in the management of peri-implant diseases. British Dental Journal, 225(5), 415-420.
[5] Isidor, F. (1997). Loss of osseointegration caused by occlusal overload of oral implants. A clinical and radiographic study in humans. Clinical Oral Implants Research, 8(2), 142-149.
Dental Implant Bruxism Risk Assessor (2026)
Use this tool to estimate your potential risk for teeth grinding dental implant damage based on common factors. This is for informational purposes only and not a substitute for professional dental advice.

Leave a Reply
Share your thoughts or ask a question about dental implants. Your email address will not be published.