Embarking on the journey of dental implant placement is a significant step towards restoring your smile and oral function. For individuals managing diabetes, this process, particularly the recovery phase, requires a tailored and meticulous approach. Successfully navigating diabetic dental implant recovery is not just about healing; it’s about optimizing systemic health to ensure the longevity and stability of your new implants. This comprehensive guide, updated for 2026, delves into the essential considerations, best practices, and expert advice to help diabetic patients achieve an optimal recovery and long-term success with their dental implants. Understanding the intricate relationship between diabetes and oral health is paramount for any patient considering or undergoing dental implant surgery.
Key Takeaways
- Blood Sugar Control is Paramount: Maintaining stable blood glucose levels before, during, and after surgery is the single most critical factor for successful diabetic dental implant recovery, directly impacting healing and reducing complication risks.
- Detailed Pre- and Post-Operative Planning: Collaborate closely with your dental surgeon and endocrinologist to develop a personalized care plan, including medication adjustments, dietary recommendations, and a strict follow-up schedule.
- Rigorous Oral Hygiene: Meticulous plaque control and the use of prescribed antimicrobial rinses are essential to prevent infection, which is a heightened risk for diabetic patients.
- Patience and Adherence: Osseointegration (the fusion of the implant with bone) takes time, and diabetic patients may require a slightly longer healing period. Adhering strictly to all post-operative instructions is non-negotiable.
- Recognize and Report Complications Promptly: Be vigilant for signs of infection, excessive bleeding, or prolonged pain, and communicate any concerns to your dental team immediately.
Understanding Diabetes and Dental Implant Success
Diabetes, a chronic metabolic condition, affects the body’s ability to process glucose, leading to high blood sugar levels. This systemic condition has profound implications for oral health, particularly when it comes to surgical procedures like dental implant placement. The success of diabetic dental implant recovery hinges significantly on how well a patient’s diabetes is managed.
High blood sugar can impair the body’s healing capabilities by affecting blood flow, reducing immune function, and altering bone metabolism. These factors can collectively increase the risk of complications such as infection, delayed healing, and even implant failure. Conversely, well-controlled diabetes—evidenced by stable HbA1c levels and consistent blood glucose readings—significantly improves the prognosis for dental implant procedures, bringing it much closer to that of non-diabetic patients [1].
How Diabetes Impacts Healing and Osseointegration
The process by which a dental implant integrates with the jawbone is called osseointegration. This is a crucial biological process that allows the implant to become a stable foundation for a prosthetic tooth. For diabetic patients, several factors can influence this process:
- Impaired Blood Flow: Chronic high blood sugar can damage blood vessels, reducing the supply of oxygen and nutrients to the surgical site, which is vital for tissue repair and bone regeneration.
- Weakened Immune Response: Diabetes can compromise the immune system, making patients more susceptible to bacterial infections, which can jeopardize the implant site.
- Altered Bone Metabolism: Diabetes can affect bone density and quality, potentially leading to slower or less robust bone formation around the implant.
- Inflammation: Diabetic individuals often experience a higher baseline of systemic inflammation, which can complicate the healing process and increase pain.
“Effective glycemic control is not merely a recommendation; it’s a prerequisite for successful dental implant integration in diabetic patients.”
These factors highlight why a collaborative approach involving the patient’s dentist, oral surgeon, and primary care physician or endocrinologist is absolutely essential for optimal outcomes. Pre-operative assessment of blood sugar levels (e.g., HbA1c test) provides valuable insights into long-term glycemic control and helps determine surgical readiness.
The Diabetic Dental Implant Recovery Timeline: What to Expect
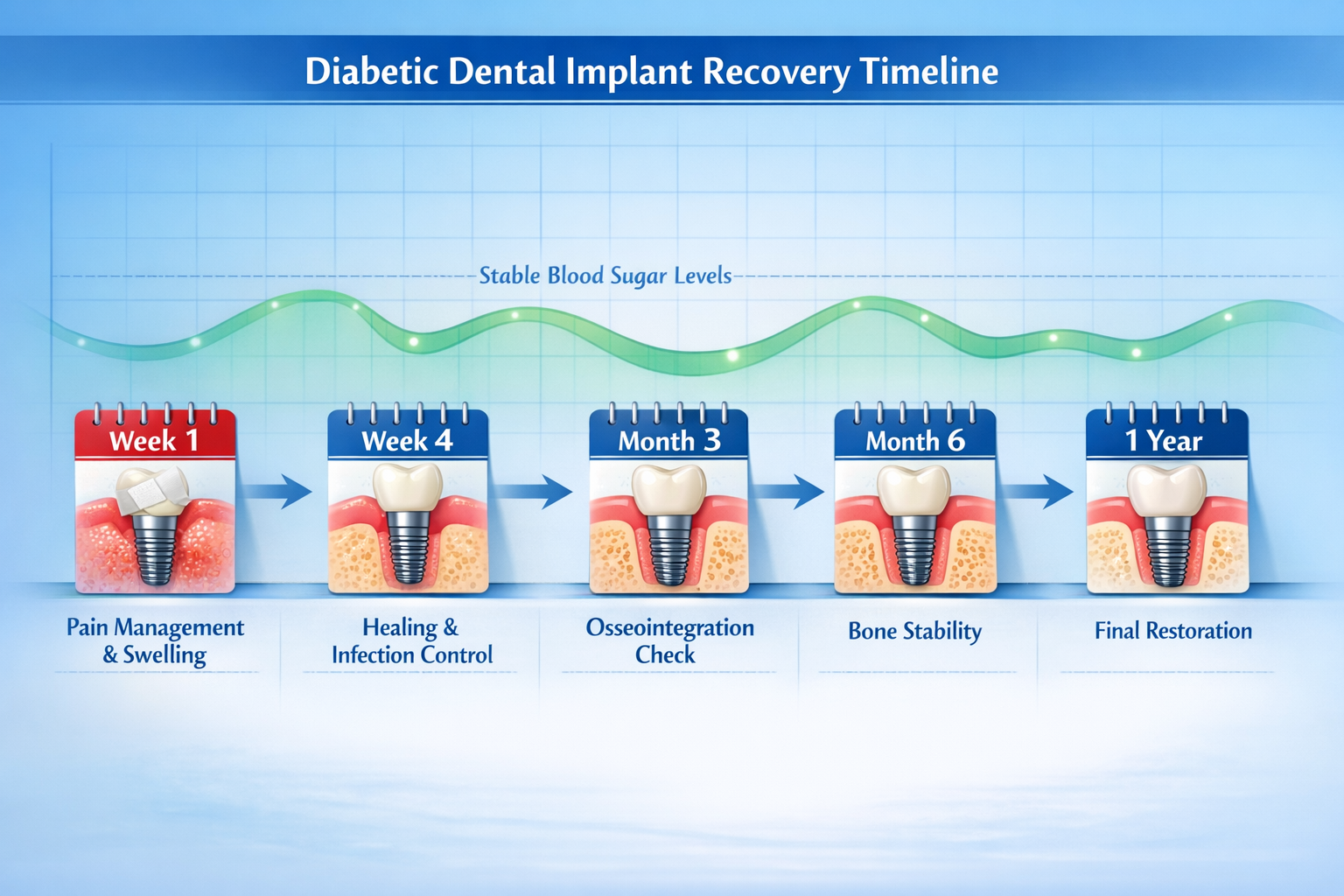
The recovery process for dental implants generally spans several months, as it involves the gradual fusion of the implant with the jawbone. For diabetic patients, this timeline might be slightly extended, and particular vigilance is required at each stage. Understanding what to expect during your diabetic dental implant recovery can help you prepare and manage your expectations. For a general overview, you might find information on a complete dental implant recovery timeline helpful, but remember to factor in the diabetic considerations discussed here.
Immediate Post-Operative Period (First Week)
The first few days after surgery are critical for initial healing and managing discomfort.
- Pain and Swelling: Expect some pain, swelling, and bruising, which can be managed with prescribed pain medication and cold compresses. Swelling usually peaks 2-3 days post-surgery.
- Bleeding: Minor bleeding or oozing is normal. Apply gentle pressure with gauze as instructed.
- Blood Sugar Monitoring: Crucially, monitor your blood sugar levels frequently. Stress from surgery can temporarily elevate glucose levels. Follow your doctor’s instructions for insulin or medication adjustments.
- Diet: Stick to soft foods that require minimal chewing. Hydration is also very important. Learn more about soft foods after dental implant surgery.
- Oral Hygiene: Gentle rinsing with a prescribed antimicrobial mouthwash is typically recommended. Avoid brushing the surgical site directly for the first 24-48 hours.
- Rest: Adequate rest is vital for recovery. Avoid strenuous activities.
Weeks 2-4: Early Healing and Osseointegration
During this phase, initial soft tissue healing occurs, and the bone-to-implant integration begins.
- Suture Removal: If non-dissolving sutures were used, they will be removed around 7-10 days post-surgery.
- Reduced Discomfort: Pain and swelling should significantly diminish.
- Continued Blood Sugar Management: Maintain diligent blood sugar control. Uncontrolled glucose at this stage can impede bone healing.
- Diet Progression: Gradually introduce more solid foods as tolerated, but still avoid hard, crunchy, or sticky items around the implant site.
- Oral Hygiene: Resume gentle brushing around the surgical area, in addition to continued rinsing. Your dentist may recommend a soft-bristled brush.
Months 2-6: Osseointegration and Abutment Placement
This is the main period for osseointegration, where the implant fuses with your jawbone. This process can take 3 to 6 months, sometimes longer for diabetic patients or those requiring bone grafting.
- Regular Check-ups: Your dental team will schedule appointments to monitor healing and assess osseointegration.
- Abutment Placement: Once osseointegration is confirmed, a minor procedure may be performed to attach the abutment – a connector piece that will hold the final crown. This is discussed in detail in guides about abutment placement and the complete guide to the dental implant abutment procedure. The healing time for the abutment is usually shorter, around 1-2 weeks.
- Final Restoration: After the abutment heals, impressions will be taken to create your custom crown, bridge, or denture, which will then be attached.
| Phase | Key Activities | Diabetic Considerations |
|---|---|---|
| Immediate (Day 1-7) | Pain/swelling management, soft diet, gentle oral hygiene, rest | Frequent blood sugar monitoring, medication adjustments, infection watch |
| Early Healing (Week 2-4) | Suture removal, diet progression, continued oral hygiene | Maintain strict glycemic control, monitor for delayed healing |
| Osseointegration (Month 2-6) | Regular dental check-ups, abutment placement, final restoration | Patience for osseointegration, continuous blood sugar management, vigilance against peri-implantitis |
Note: This timeline is a general guide. Your individual recovery may vary based on your overall health, the number of implants, and any additional procedures like bone grafting.
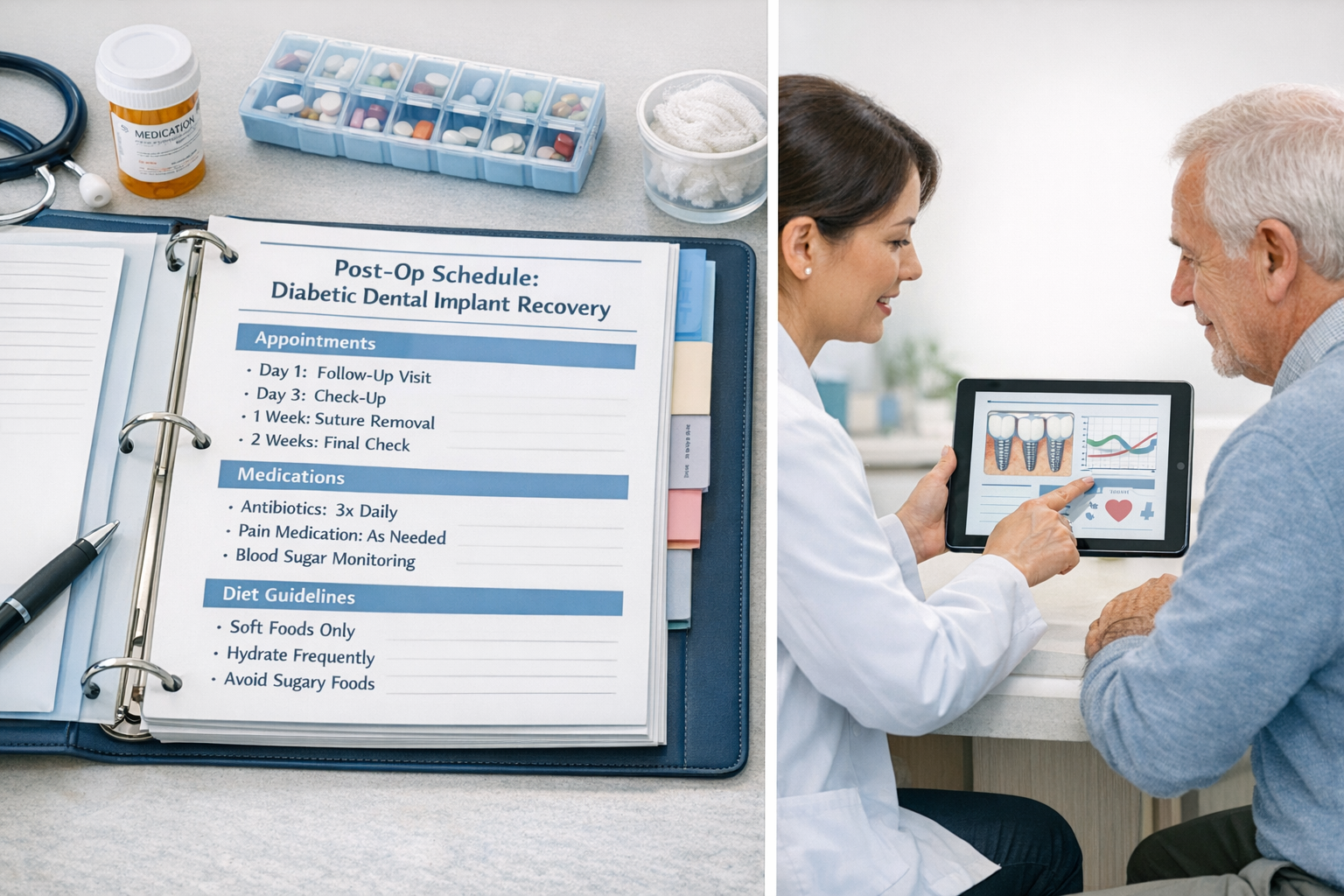
Critical Post-Operative Care for Diabetic Patients

Meticulous post-operative care is non-negotiable for successful diabetic dental implant recovery. It involves a multi-faceted approach addressing both oral hygiene and systemic health management.
Blood Glucose Control: The Foundation of Healing
As emphasized, maintaining stable blood glucose levels is the cornerstone of successful recovery.
- Pre-Surgery: Your doctor will likely recommend ensuring your HbA1c is below a certain threshold (often <7-8%) before surgery [2].
- Post-Surgery:
- Frequent Monitoring: Check your blood sugar more often than usual, especially during the first few days.
- Medication Adherence: Take all diabetes medications as prescribed. Do not skip doses, even if your diet changes.
- Communicate with Your Doctor: Report any significant or persistent fluctuations in blood sugar to your endocrinologist or primary care physician. They may need to adjust your medication temporarily.
- Healthy Eating: Continue to follow a diabetic-friendly diet, adapting it to soft foods initially. Avoid sugary drinks and processed foods that can spike glucose levels.
Oral Hygiene: Preventing Infection and Promoting Healing
Diabetic patients are at a higher risk of oral infections due to compromised immune function and slower healing. Therefore, impeccable oral hygiene is paramount.
- Gentle Brushing: After the initial 24-48 hours, gently brush your teeth, avoiding the surgical site. Once cleared by your dentist, carefully clean around the implant with a soft-bristled brush.
- Antimicrobial Rinses: Use a prescribed chlorhexidine gluconate mouthwash as directed. This helps reduce bacteria in your mouth and prevents infection. Avoid alcohol-based mouthwashes, which can be irritating.
- Water Flossing: Once healing has progressed, a water flosser can be an effective tool for cleaning around implants, but always use it on the lowest setting and only after your dentist advises it. Many find a best water flosser for dental implants to be a valuable investment.
- Avoid Irritants: Refrain from smoking, consuming alcohol, or using straws, as these can disrupt the healing clot and introduce bacteria. Smoking is particularly detrimental, as discussed in contexts like after root canal can you smoke, and the risks are even higher for implant recovery. Similarly, alcohol after dental implant surgery should be avoided.
Medication Management
Your dental surgeon will prescribe medications to manage pain and prevent infection.
- Antibiotics: Take the full course of prescribed antibiotics, even if you feel better. This is crucial for preventing infection, which is a major concern for diabetic patients. Understanding the role of antibiotics after dental implant surgery is vital.
- Pain Relievers: Use pain medication as directed. Do not exceed the recommended dose.
- Anti-Inflammatories: If prescribed, these can help reduce swelling and discomfort.
Dietary Adjustments
Proper nutrition supports healing and helps maintain blood sugar stability.
- Soft Food Diet: For the first few days to weeks, stick to soft, nutrient-dense foods. Examples include mashed potatoes, yogurt, smoothies, cooked cereals, and pureed soups.
- Avoid: Hard, crunchy, spicy, acidic, or very hot foods, which can irritate the surgical site.
- Hydration: Drink plenty of water to stay hydrated and aid recovery.
Potential Complications and How to Mitigate Risks
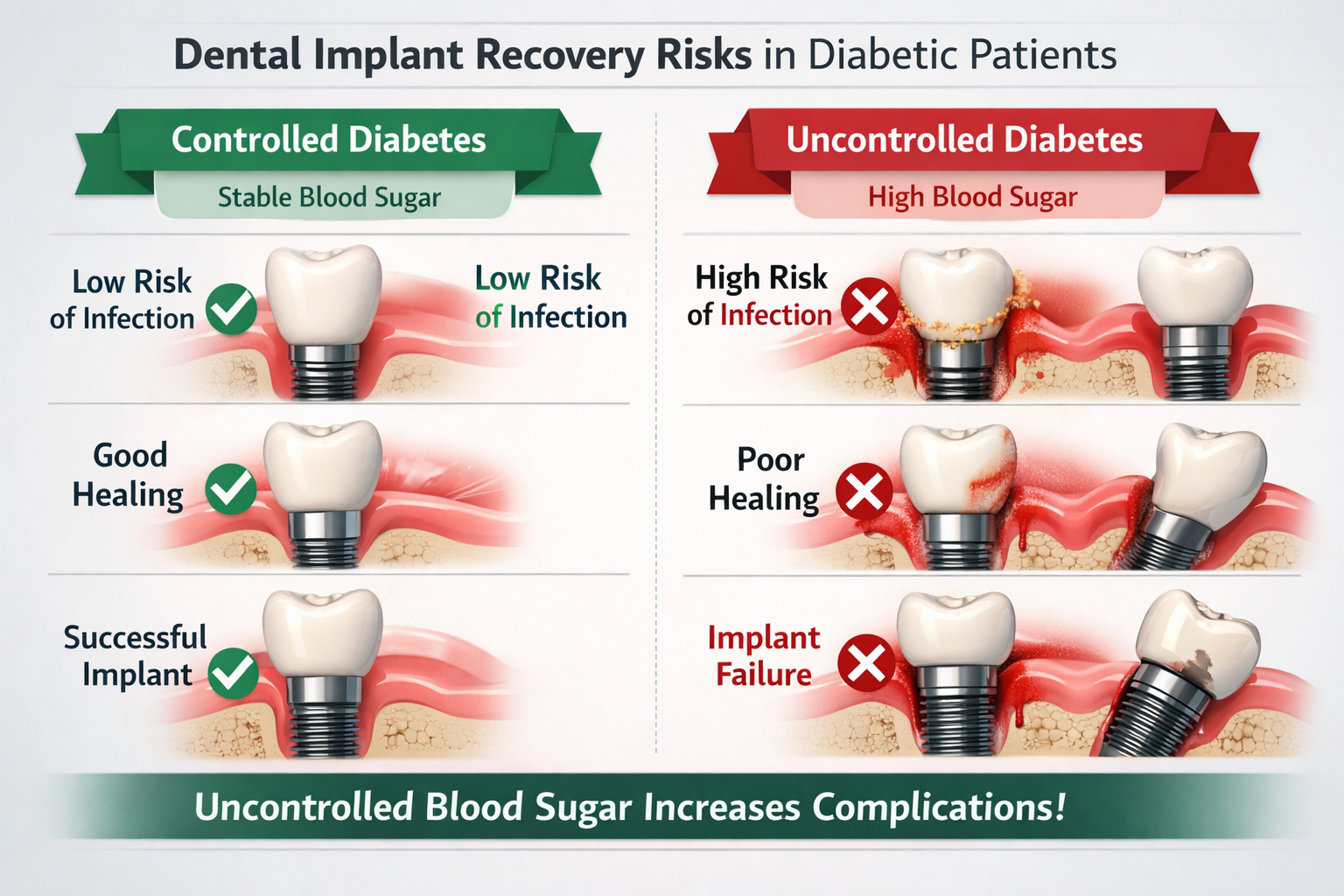
While dental implants boast high success rates, diabetic patients face a slightly elevated risk of certain complications during diabetic dental implant recovery. Awareness and proactive management are key to mitigating these risks.
Increased Risk of Infection
Diabetic patients have a higher propensity for infections due to impaired immune function.
- Mitigation: Strict adherence to antibiotic regimens, meticulous oral hygiene, and, most importantly, tight blood glucose control. Any signs of infection (persistent pain, swelling, pus, fever) should be reported immediately.
Delayed Healing and Osseointegration
The bone healing process can be slower in diabetic individuals.
- Mitigation: Patience is crucial. Maintaining optimal blood sugar levels consistently will greatly support bone healing. Your dental team may also recommend a longer healing period before placing the final restoration. Regular follow-up appointments allow your dentist to monitor progress.
Peri-Implantitis
This is an inflammatory condition affecting the soft and hard tissues surrounding a dental implant, often leading to bone loss and potential implant failure if untreated. It’s akin to periodontal disease around natural teeth, and diabetic patients are more susceptible [3].
- Mitigation: Exemplary long-term oral hygiene, regular professional cleanings specific for implants, and ongoing diabetic control are essential. Early detection and treatment are vital.
Implant Failure
Although rare, implant failure can occur if osseointegration does not happen or if complications arise.
- Mitigation: The most significant factor in preventing implant failure for diabetic patients is stringent glycemic control. Choosing an experienced dental implant specialist, ensuring comprehensive pre-operative assessment, and following all post-operative instructions diligently also play crucial roles. This comprehensive care is why finding the best dental implant centers is so important.
Table of Risk Mitigation Strategies
| Risk Category | Specific Risks for Diabetics | Mitigation Strategies |
|---|---|---|
| Infection | Post-operative infection, abscess | Strict antibiotics, antiseptic rinses, impeccable oral hygiene, tight blood glucose control |
| Healing Impairment | Delayed osseointegration, poor soft tissue healing | Consistent blood sugar management, nutrient-rich diet, adequate rest, patience for healing periods |
| Long-Term Complications | Peri-implantitis, implant failure | Lifelong meticulous oral hygiene, regular dental check-ups, professional implant cleanings, ongoing diabetes management |
| Surgical Complications | Excessive bleeding | Pre-operative communication with medical doctor about blood thinners, careful surgical technique |
Long-Term Maintenance and Ongoing Diabetes Management
Successful diabetic dental implant recovery extends far beyond the initial healing phase. Long-term maintenance and unwavering commitment to diabetes management are fundamental to ensuring the longevity and health of your dental implants. Consider your implants an investment that requires continuous care, much like managing your diabetes itself.
Regular Dental Check-ups and Professional Cleanings
Even with implants, regular dental visits are crucial.
- Specialized Care: Your dental hygienist should be trained in caring for dental implants. They will use specialized tools that won’t scratch the implant surface and will check for any signs of inflammation or issues around the implants.
- Frequency: Typically, professional cleanings are recommended every 3-6 months, though your dentist may suggest a more frequent schedule based on your oral health and diabetic status. These professional cleanings are key to preventing peri-implantitis and other issues.
- Early Detection: Regular check-ups allow your dental team to detect and address potential problems early, before they escalate.
Continued Optimal Oral Hygiene Practices
The habits you develop during recovery must become a lifelong routine.
- Brushing and Flossing: Continue to brush twice daily with a soft-bristled brush and use interdental brushes or a water flosser to clean around the implant posts.
- Antimicrobial Rinses: Your dentist might recommend periodic use of antimicrobial rinses, especially if you show signs of inflammation or have difficulty with plaque control.
- Self-Monitoring: Be vigilant for any changes in your gums around the implants, such as redness, swelling, or bleeding, and report them to your dentist.
Consistent Diabetes Management
Your implants’ long-term success is inextricably linked to your overall health and, specifically, your diabetes management.
- Adhere to Medical Advice: Continue to follow your primary care physician’s or endocrinologist’s advice regarding diet, exercise, and medication for diabetes control.
- Monitor HbA1c: Regular monitoring of your HbA1c levels provides a clear picture of your long-term blood sugar control, which is a strong predictor of implant success.
- Healthy Lifestyle: A balanced diet, regular physical activity, and avoiding smoking are beneficial for both your diabetes and your oral health. Smoking, in particular, significantly increases the risk of implant complications and failure.
By integrating these long-term strategies into your daily life, you can significantly enhance the success and durability of your dental implants, allowing you to enjoy a restored smile and improved quality of life for years to come. For more information about the clinic’s commitment to patient success, you can visit their about us page.
Diabetic Dental Implant Recovery Checklist 💡
✅ Use this interactive checklist to track your progress during diabetic dental implant recovery. Mark off items as you complete them, and remember that consistent adherence to these steps is key to success!
Conclusion
Achieving successful diabetic dental implant recovery is a journey that demands diligence, collaboration, and a thorough understanding of the unique challenges and strategies involved. For individuals managing diabetes in 2026, the prospect of dental implants offers a transformative solution for tooth replacement, but it comes with a heightened responsibility for self-care and adherence to professional guidance.
From meticulous blood glucose control to unwavering oral hygiene and regular professional check-ups, every step plays a pivotal role in ensuring the successful integration and longevity of your dental implants. By embracing a proactive approach, maintaining open communication with your dental and medical teams, and committing to a healthy lifestyle, diabetic patients can confidently navigate the recovery process and enjoy the profound benefits of a restored smile and improved oral health. The journey requires patience and consistent effort, but the rewards of a functional and aesthetic dental restoration are well worth it.
Actionable Next Steps:
- Consult Your Healthcare Team: Before any dental implant procedure, have a detailed discussion with your endocrinologist/PCP and dental surgeon to ensure your diabetes is well-controlled and a personalized treatment plan is in place.
- Understand Your Instructions: Fully comprehend all pre- and post-operative instructions, especially regarding medications, diet, and oral hygiene. Ask questions if anything is unclear.
- Prioritize Blood Sugar Monitoring: Make frequent blood glucose monitoring a top priority throughout your recovery. Report any significant changes to your medical doctor.
- Commit to Oral Hygiene: Implement and maintain a rigorous oral hygiene routine, including gentle brushing and using any prescribed rinses, as a lifelong habit.
- Attend All Follow-ups: Do not miss any scheduled dental appointments, as these are vital for monitoring healing and ensuring the long-term success of your implants.
Remember, your health is a partnership. By actively participating in your care and staying informed, you significantly increase the likelihood of a smooth diabetic dental implant recovery and the lasting success of your new smile.
References
[1] Al-Mishriky, A. A., & Al-Amry, M. A. (2019). The Success Rate of Dental Implants in Patients with Controlled Versus Uncontrolled Diabetes Mellitus: A Systematic Review. Journal of Clinical and Diagnostic Research, 13(7), ZC01-ZC04.
[2] American Academy of Periodontology. (2018). Periodontal Disease and Diabetes. Retrieved from https://www.perio.org/consumer/diabetes.htm (Note: While not directly citing implants, it reinforces the link between diabetes control and oral health.)
[3] Ata-Ali, J., & Ata-Ali, F. (2015). Do diabetic patients have a higher risk of dental implant failure? A meta-analysis. Medicina Oral, Patología Oral y Cirugía Bucal, 20(4), e467-e471.

Leave a Reply
Share your thoughts or ask a question about dental implants. Your email address will not be published.