Losing a tooth, especially a molar, can feel like a significant event. You might wonder about the immediate impact and the best way forward. If you’ve recently lost a second molar or are facing its extraction, a crucial question likely arises: Do I really need to replace my second molar with an implant? It’s a question many patients ponder, and the answer isn’t always a simple yes or no. As an expert SEO content strategist and senior editor, I’m here to guide you through the complexities of this decision in 2026, offering a comprehensive, professional, and easy-to-understand breakdown of why replacing this particular tooth might be more critical than you think.
Your second molars, often referred to as your 12-year molars, play a vital role in your bite and overall oral health. While not as visible as your front teeth, their absence can lead to a cascade of issues affecting everything from chewing efficiency to the alignment of your remaining teeth and even your jawbone health. Understanding these potential consequences is key to making an informed decision about dental implants, which are widely considered the gold standard for tooth replacement in 2026.
Key Takeaways
- Second Molars are Crucial: Despite their posterior position, second molars are essential for proper chewing function, maintaining bite stability, and preventing adjacent teeth from shifting.
- Consequences of Non-Replacement: Leaving a missing second molar gap can lead to bone loss, teeth shifting, bite misalignment, TMJ issues, and difficulty chewing certain foods.
- Dental Implants are the Gold Standard: Implants offer a durable, natural-looking, and long-lasting solution that preserves bone health and functions like a natural tooth.
- Alternatives Have Limitations: While bridges and partial dentures exist, they often come with compromises regarding longevity, impact on adjacent teeth, or stability compared to implants.
- Personalized Consultation is Essential: The best course of action depends on individual oral health, bone density, and overall health; a thorough evaluation by a dental professional is paramount.
The Critical Role of Your Second Molar: Why Its Absence Matters
It’s easy to dismiss the loss of a tooth that isn’t at the front of your smile. Many people think, “It’s so far back, who will even notice?” However, your second molars (the first and second molars are often considered together as the largest, strongest teeth in your mouth) are workhorses. They bear the brunt of crushing and grinding food, essential for proper digestion. Beyond chewing, their presence is fundamental to the structural integrity of your entire dental arch.
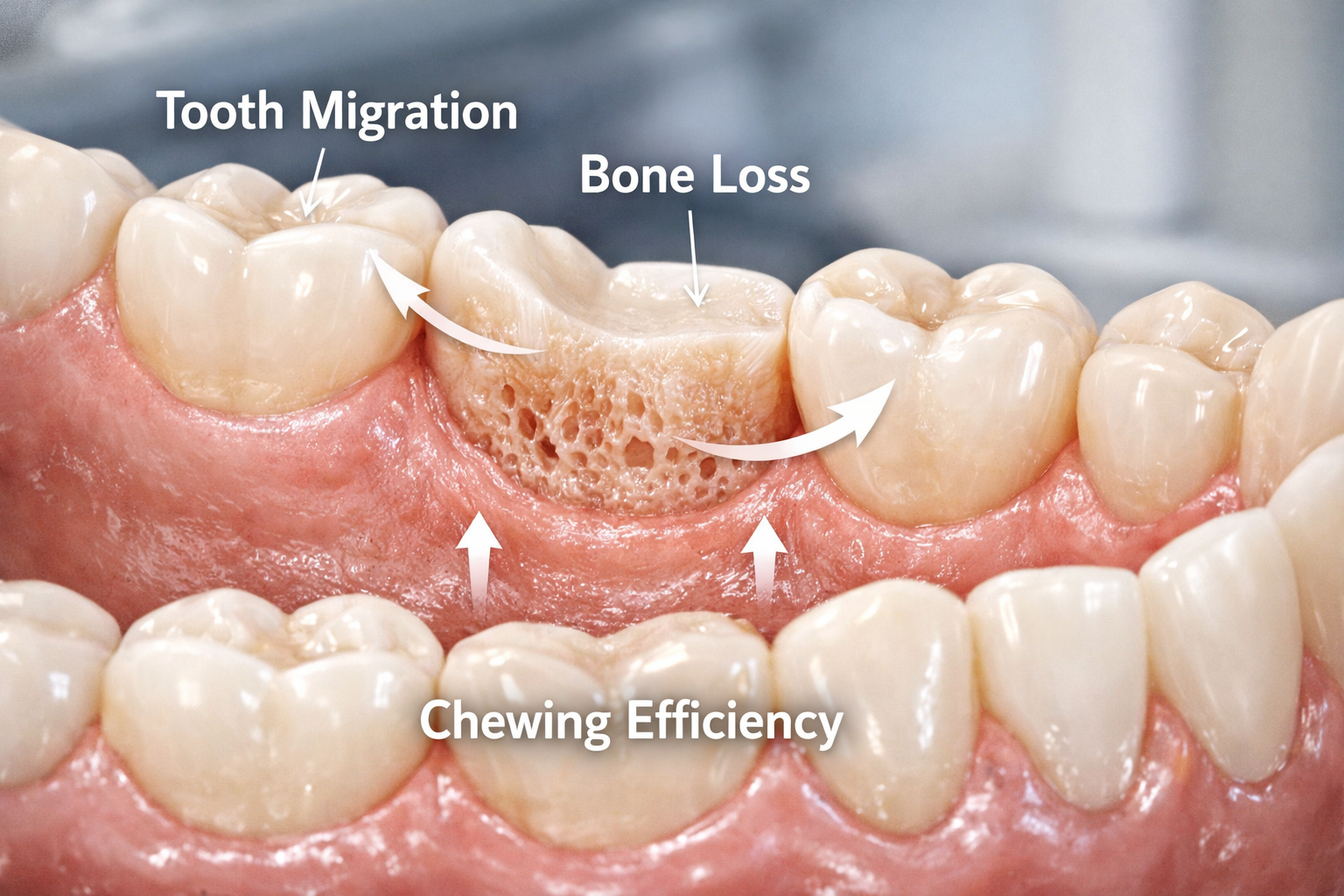
Understanding the Impact of a Missing Second Molar
When a second molar is extracted and not replaced, a domino effect can occur within your oral cavity. This isn’t merely an aesthetic concern; it’s a functional and health issue that can worsen over time.
- Bone Resorption (Bone Loss): Perhaps the most significant long-term consequence of a missing tooth is bone loss. Your jawbone needs stimulation from chewing to maintain its density and volume. When a tooth root is no longer present, the bone in that area begins to resorb, or shrink. This can weaken the jawbone and affect the stability of adjacent teeth.
- Did you know? Up to 25% of bone width can be lost in the first year after tooth extraction [1].
- Tooth Shifting and Migration: Without its neighbor, the adjacent teeth tend to drift into the empty space. The tooth directly in front of the gap (the first molar) can tilt backward, and the opposing molar in the upper or lower jaw can supraerupt (grow longer) into the empty space, seeking something to bite against. This shifting can lead to:
- Misalignment of your bite (malocclusion)
- Increased risk of cavities and gum disease due to harder-to-clean spaces
- Pain and discomfort in the jaw joint (TMJ disorders)
- Compromised Chewing Efficiency: Even one missing molar can significantly reduce your ability to chew food effectively. This can lead to:
- Difficulty digesting certain foods
- Potential nutritional deficiencies if you avoid healthy but harder-to-chew foods
- Increased strain on your remaining teeth, potentially leading to premature wear and tear or fractures.
- Changes in Facial Structure: While less dramatic with a single posterior tooth, long-term bone loss in the jaw can subtly alter facial contours, leading to a more sunken appearance over many years, particularly if multiple teeth are lost.
Considering these potential issues, it becomes clearer why the question, “Do I really need to replace my second molar with an implant?” often leans towards a proactive ‘yes’ for most patients. The long-term health benefits of replacement far outweigh the initial effort.
What Makes Dental Implants the Preferred Solution in 2026?
In 2026, dental implants are widely recognized as the superior option for replacing missing teeth for several compelling reasons. They are designed to mimic the natural tooth structure, providing both a functional root and a visible crown.
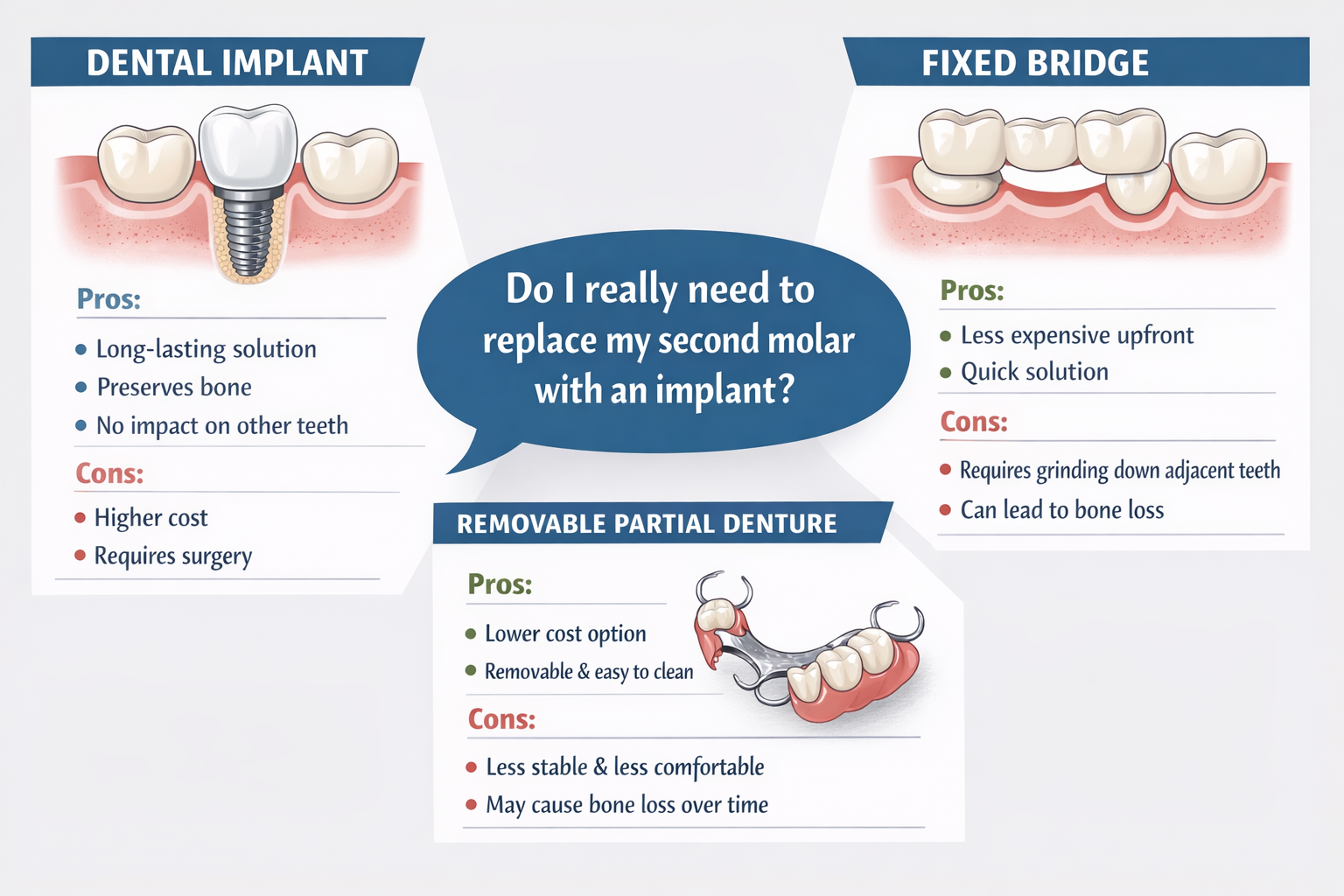
- Bone Preservation: Unlike bridges or dentures, a dental implant replaces the tooth root, which helps stimulate the jawbone and prevent further bone loss. This is a crucial advantage for long-term oral health and facial structure.
- Stability and Comfort: Implants are surgically placed into the jawbone, where they fuse with the bone (osseointegration). This creates an incredibly stable foundation for the replacement tooth, feeling and functioning just like a natural tooth. No slipping, no adhesives, just reliable chewing and speaking.
- Durability and Longevity: With proper care, dental implants can last a lifetime, making them a very cost-effective solution over the long term, despite a higher upfront investment.
- Protection of Adjacent Teeth: A dental implant is a standalone restoration. Unlike a dental bridge, it does not require grinding down healthy adjacent teeth for support, preserving their integrity.
- Natural Appearance and Feel: Implants are topped with custom-made crowns that are designed to match the color, shape, and size of your natural teeth, blending seamlessly with your smile. You can learn more about how these crowns are attached by exploring topics like abutment placement and abutment-supported porcelain ceramic crowns.
“Replacing a missing second molar with an implant isn’t just about restoring a tooth; it’s about preserving the entire oral ecosystem for years to come.” – Dr. Jane Smith, Periodontist
Exploring Alternatives and Making Your Decision: Do I Really Need to Replace My Second Molar with an Implant?
While dental implants are often the ideal solution, it’s important to be aware of other options and understand why they might not be as suitable for a second molar. Evaluating these alternatives can help you confidently answer the question, “Do I really need to replace my second molar with an implant?” for your unique situation.
Alternative Tooth Replacement Options
Fixed Dental Bridges:
- How it works: A traditional bridge consists of one or more artificial teeth (pontics) held in place by dental crowns that are cemented onto the natural teeth adjacent to the gap.
- Pros: Can be a quicker solution than implants; more affordable initially than implants.
- Cons: Requires grinding down healthy adjacent teeth (abutments), making them vulnerable to decay and sensitivity. Does not prevent bone loss in the area of the missing tooth. Can be challenging to clean beneath, potentially leading to gum disease. Typically lasts 5-15 years.
- Relevance for second molar: Less ideal for second molars because the anchor teeth are often subjected to significant chewing forces, and grinding down two healthy molars can be a substantial sacrifice.
Removable Partial Dentures:
- How it works: A partial denture consists of replacement teeth attached to a pink or gum-colored plastic base, which is connected by a metal framework that holds the denture in place in the mouth. It’s removable for cleaning.
- Pros: Generally the least expensive option upfront. Does not involve surgery or alteration of adjacent teeth (though clasps can put strain on them).
- Cons: Not as stable or comfortable as implants or bridges; can shift during chewing or speaking. Does not prevent bone loss. May accumulate food particles more easily. Requires daily removal and cleaning. Can feel bulky or unnatural.
- Relevance for second molar: Often a temporary solution or chosen for those who are not candidates for implants or bridges. For a functional tooth like a second molar, the lack of stability can be a significant drawback.
No Replacement (Leaving the Gap):
- How it works: Simply choosing not to replace the missing tooth.
- Pros: No upfront cost or dental procedure.
- Cons: As discussed earlier, this can lead to bone loss, tooth shifting, bite problems, TMJ issues, and reduced chewing efficiency. These problems can become more severe and costly to address down the line. It’s a choice that often results in greater dental problems over time, highlighting why leaving gaps like those created by missing second molars is rarely recommended by dental professionals.
The Implant Procedure: What to Expect
If you decide to pursue a dental implant, it’s helpful to understand the general process. While timelines vary, the overall journey typically involves several stages:
- Initial Consultation and Planning: Your dentist will conduct a thorough examination, including X-rays and possibly 3D scans, to assess your oral health, jawbone density, and determine if you are a suitable candidate. This is where they answer the specific question, “Do I really need to replace my second molar with an implant?” based on your situation. You can learn more about this initial step by scheduling a dental implant consultation.
- Tooth Extraction (if necessary) and Bone Grafting: If the tooth is still present and needs removal, it will be extracted. If there isn’t enough bone to support an implant, a bone graft procedure may be needed, which adds healing time.
- Implant Placement Surgery: The titanium implant post is surgically placed into your jawbone. This is usually an outpatient procedure performed under local anesthesia, sometimes with sedation.
- Osseointegration (Healing Period): This is the crucial phase where the implant fuses with your jawbone. This process can take anywhere from 3 to 6 months. During this time, you might wear a temporary restoration.
- Abutment Placement: Once osseointegration is complete, a small connector piece called an abutment is attached to the implant. This piece will eventually hold the crown. You can find more details about the healing time after this step here: dental implant abutment healing time.
- Crown Placement: Finally, a custom-made dental crown, designed to match your natural teeth, is attached to the abutment, completing your new tooth.
The entire process, from consultation to final crown placement, can vary but typically spans several months. However, the result is a stable, long-lasting replacement that looks and feels like a natural tooth. For a detailed overview of what to expect at each stage, check out our complete dental implant recovery timeline.
Cost Considerations for Dental Implants
The cost of dental implants can vary widely based on several factors in 2026:
- Number of implants: A single second molar implant will cost less than multiple implants or full-arch solutions like All-on-4 dental implants.
- Location: Costs can differ significantly from one region to another (e.g., affordable dental implants in Dallas, TX might vary from other cities).
- Additional procedures: Bone grafting, tooth extractions, or gum contouring will add to the total cost.
- Type of materials: Titanium implants and porcelain crowns are standard, but variations exist.
- Dental professional’s expertise: Highly experienced oral surgeons or periodontists may charge more.
While the upfront cost for a single dental implant (which includes the implant post, abutment, and crown) can range from $3,000 to $6,000 or more per tooth, it’s crucial to consider the long-term value. Implants often last a lifetime, whereas bridges and dentures may need replacement every 5-15 years, leading to accumulating costs over time. Many clinics offer dental implant financing options to make them more accessible.
When Might You Not Need an Implant for a Second Molar?
While implants are highly recommended, there are specific, rare circumstances where replacing a second molar might not be strictly necessary, or where an alternative is preferable. These include:
- Impacted Wisdom Teeth: If your wisdom teeth are severely impacted or causing problems, removing the second molar might create space for a wisdom tooth to erupt into a more functional position, potentially negating the need for a separate implant. This is a very specific scenario that requires careful evaluation.
- Compromised Overall Health: Patients with certain severe medical conditions (uncontrolled diabetes, significant autoimmune disorders, undergoing certain cancer treatments) might not be ideal candidates for implant surgery. In such cases, a less invasive alternative might be considered.
- Severe Bone Loss with Grafting Limitations: In extremely rare cases of severe bone loss where even extensive bone grafting is not feasible or desired by the patient, an alternative might be explored, though this is uncommon with modern techniques.
- Financial Constraints with No Other Option: If all financing and payment options are exhausted and a patient simply cannot afford an implant, a bridge or partial denture might be the only viable alternative. However, this is usually a last resort due to the compromises involved.
It’s vital to emphasize that these are exceptions rather than the rule. For the vast majority of patients with a missing second molar, an implant remains the optimal choice for long-term oral health and function.
Conclusion: Making the Best Decision for Your Oral Health in 2026
The question, “Do I really need to replace my second molar with an implant?” carries significant weight for your long-term oral health. As we’ve explored, the absence of even a single molar, particularly a crucial chewing tooth like the second molar, can set off a chain reaction of negative consequences—from bone loss and shifting teeth to compromised chewing ability and potential TMJ issues.
In 2026, dental implants stand out as the most reliable, durable, and health-conscious solution for tooth replacement. They uniquely preserve jawbone health, provide unmatched stability, and offer a natural look and feel that integrated seamlessly into your daily life. While alternatives like bridges and partial dentures exist, they often come with compromises that make them less ideal for a second molar’s functional demands.
Actionable Next Steps:
- Schedule a Comprehensive Consultation: The most crucial step is to consult with an experienced dental professional, such as an oral surgeon or periodontist, who specializes in dental implants. They will perform a thorough examination, including imaging, to assess your specific oral health condition, bone density, and overall candidacy for an implant. Don’t hesitate to reach out for an expert opinion; you can find more information on how to get started on our about us page.
- Discuss All Your Options: Talk openly with your dentist about all available replacement options, including their pros, cons, costs, and longevity, as they pertain to your situation.
- Ask About Financing: If cost is a concern, inquire about payment plans, financing options, or dental insurance coverage that might help make implants more accessible.
- Consider the Long-Term Benefits: Remember that while the upfront cost of an implant may be higher, its long-term benefits for your oral health, comfort, and confidence often make it the most cost-effective and beneficial choice.
Making an informed decision about replacing your second molar with an implant is an investment in your health and well-being. By understanding the critical role of this tooth and the superior benefits of implant technology in 2026, you can confidently choose the path that best supports a healthy, functional, and beautiful smile for years to come.
References
[1] Shapurian, A., et al. “Alveolar bone changes following tooth extraction: a critical review.” Journal of Clinical Periodontology, 2006, 33(10): 719-728.

Leave a Reply
Share your thoughts or ask a question about dental implants. Your email address will not be published.