Embarking on the journey to restore your smile with dental implants is a significant step towards improved oral health and confidence. However, the success and longevity of your new teeth largely depend on understanding and meticulously managing the dental implants healing process. This period, often underestimated, is crucial for the implant to integrate properly with your jawbone. As an expert in dental care, I’m here to guide you through every stage of healing, helping you navigate the expectations, best practices, and potential challenges you might encounter in 2026. From the immediate post-surgery care to the long-term maintenance, this article will equip you with the knowledge needed to ensure a smooth and successful recovery.
Key Takeaways
- Phased Healing Process: Dental implant healing involves distinct stages: initial recovery, osseointegration, and abutment/crown placement, each with specific requirements.
- Osseointegration is Crucial: The most vital part of healing is osseointegration, where the implant fuses with your jawbone, typically taking 3-6 months.
- Diligent Aftercare is Essential: Following post-operative instructions, including diet modifications, oral hygiene, and avoiding harmful habits, significantly impacts success.
- Potential Complications Exist: While rare, complications like infection, implant failure, or nerve damage can occur, making regular follow-ups with your dentist paramount.
- Long-Term Success through Maintenance: Proper oral hygiene and routine dental check-ups are key to ensuring the longevity of your dental implants for years to come.
Understanding the Initial Stages of Dental Implants Healing

The moment your dental implant is placed, a remarkable biological process begins. The initial stages of dental implants healing are critical and set the foundation for the implant’s long-term success. This phase typically covers the first few days to weeks following your surgery.
Immediate Post-Surgery: The First 24-72 Hours
The first few days after your dental implant surgery are when you’ll experience the most noticeable symptoms and require the most careful attention. My team and I always emphasize that patients must strictly adhere to the post-operative instructions provided to minimize discomfort and prevent complications.
What to Expect:
- Bleeding: Some light bleeding or oozing from the surgical site is normal. You’ll likely be instructed to bite down on gauze pads, changing them as needed. This helps to form a blood clot, which is vital for healing.
- Swelling: Swelling around the surgical area is common and usually peaks within 48-72 hours. Applying ice packs to the outside of your cheek for 20 minutes on, 20 minutes off, can help reduce swelling and discomfort.
- Pain/Discomfort: You will experience some pain, but it should be manageable. Your dentist will prescribe pain medication or recommend over-the-counter options. Taking medication as directed is crucial for comfort.
- Diet Restrictions: A soft-food diet is essential. Avoid chewing directly on the implant site. Think smoothies, soups, yogurt, and mashed potatoes. For a detailed list of safe options, you can refer to our guide on 50 soft foods after dental implant.
- Oral Hygiene: Gentle oral hygiene is paramount. You might be instructed to use a special antimicrobial mouthwash or perform very gentle saltwater rinses after the initial 24 hours. Avoid vigorous rinsing, spitting, or using straws, as these can dislodge the crucial blood clot.
Key Actions for the First Few Days:
- Rest: Elevate your head with pillows while resting or sleeping to help reduce swelling.
- Hydrate: Drink plenty of fluids, but avoid alcohol and sugary drinks.
- Avoid Smoking: Smoking severely impedes healing and significantly increases the risk of implant failure. If you’re a smoker, this is a critical time to abstain.
The First Week and Beyond: Initial Soft Tissue Healing
As the immediate post-operative period subsides, your focus shifts to the healing of the soft tissues (gums) around the implant site.
- Sutures: If sutures were used, they might dissolve on their own or require removal by your dentist, typically within 7-10 days.
- Decreased Swelling and Pain: You should notice a significant reduction in swelling and pain. If pain worsens or swelling persists beyond a few days, contact your dentist immediately.
- Continued Soft Diet: While you might feel better, continue with a soft diet for at least the first week, gradually introducing more solid foods as advised by your dentist.
- Gentle Oral Hygiene: Continue with very gentle brushing around the surgical site, being careful not to disturb the healing tissues. Your dentist may recommend a specialized soft-bristle brush.
“The first week after dental implant surgery is pivotal. Following all instructions carefully lays the groundwork for successful osseointegration.”
Osseointegration: The Core of Dental Implants Healing
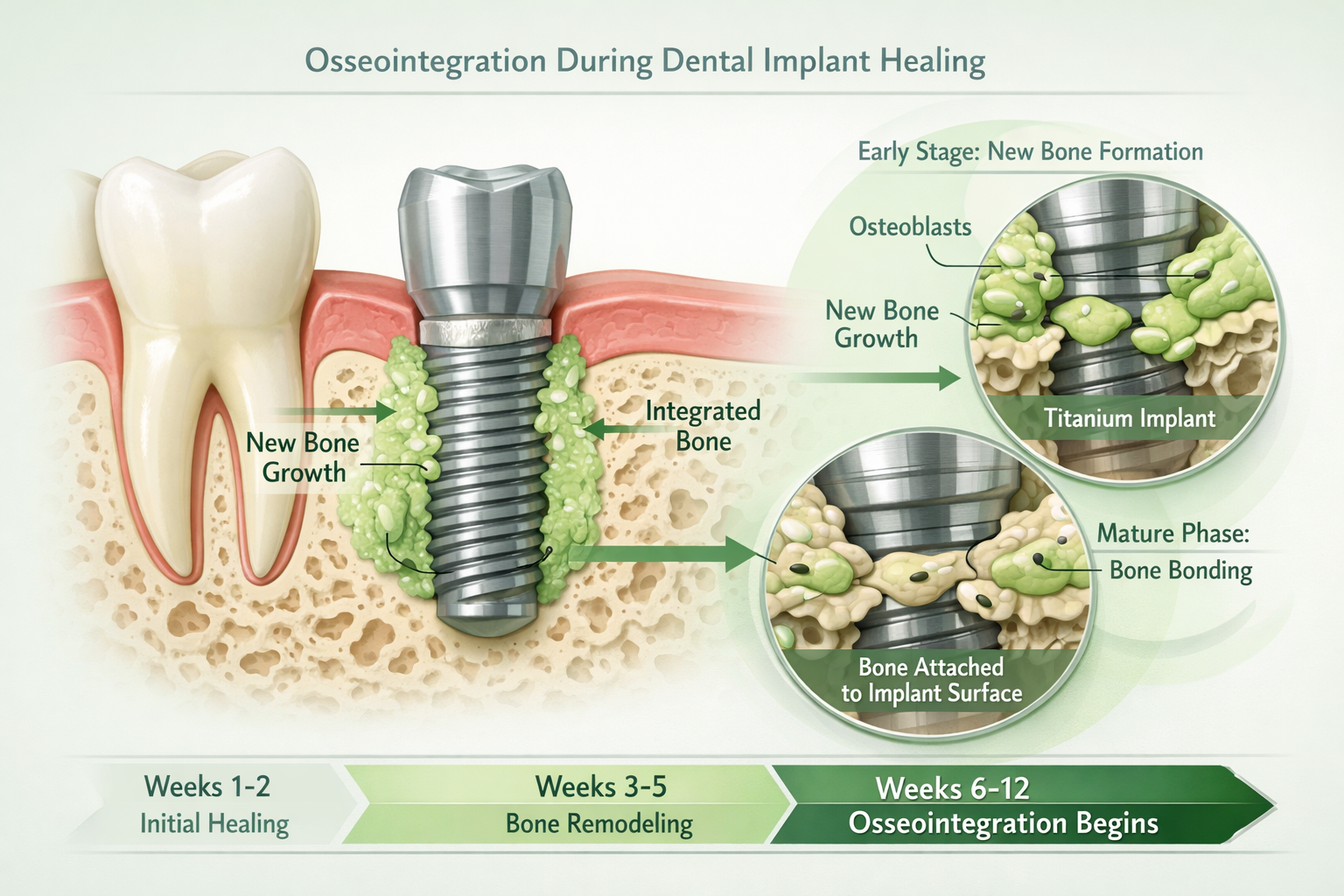
The term “osseointegration” is central to the success of dental implants. It refers to the process where the bone cells of your jaw directly grow onto and fuse with the surface of the titanium implant. This biological bond creates a strong, stable foundation for your future crown, bridge, or denture.
The Science Behind the Fusion
Titanium, the material used for most dental implants, is remarkably biocompatible. This means your body recognizes it as a natural component and doesn’t reject it. Once the implant is placed into the jawbone, a complex biological cascade begins:
- Blood Clot Formation: Immediately after placement, a blood clot forms around the implant, bringing growth factors and cells essential for healing.
- Bone Growth: Specialized bone cells (osteoblasts) migrate to the implant surface and begin laying down new bone tissue.
- Remodeling: Over time, this new bone matures and strengthens, creating a direct structural and functional connection between the living bone and the surface of the implant.
The Osseointegration Timeline
The duration of osseointegration varies from person to person, influenced by factors like bone quality, implant location, overall health, and whether a bone graft was performed.
| Factor | Typical Healing Time (Osseointegration) | Notes |
|---|---|---|
| Lower Jaw | 3-4 months | Generally denser bone, faster healing. |
| Upper Jaw | 4-6 months | Bone in the upper jaw (maxilla) is often less dense, requiring a longer healing period. |
| Bone Grafting | Additional 4-9 months | If a bone graft was needed before or during implant placement, this significantly extends total time. |
| Individual Health | Varies | Smokers, diabetics, and those with certain medical conditions may experience longer healing. |
It’s crucial to understand that during this entire period, the implant should not be subjected to significant chewing forces. This “unloaded” state allows the delicate bone-implant interface to form without disruption. Rushing this stage can lead to implant failure. Your dentist will monitor your progress with X-rays to confirm successful osseointegration before proceeding to the next steps.
What Happens After Osseointegration?
Once your implant has fully integrated, the next phase is typically the placement of the abutment. An abutment is a small connector piece that screws into the dental implant and protrudes through the gum line, serving as the base for your final crown or prosthesis. This procedure is generally minor and has its own dental implant abutment healing time. After the abutment heals, your custom-made crown (like an abutment-supported porcelain ceramic crown) will be attached, completing your new tooth.
Managing Challenges and Ensuring Success During Dental Implants Healing
While the majority of dental implant procedures are highly successful, understanding potential challenges and how to mitigate them is a crucial part of the dental implants healing process. Being informed allows you to recognize signs of concern early and take appropriate action.
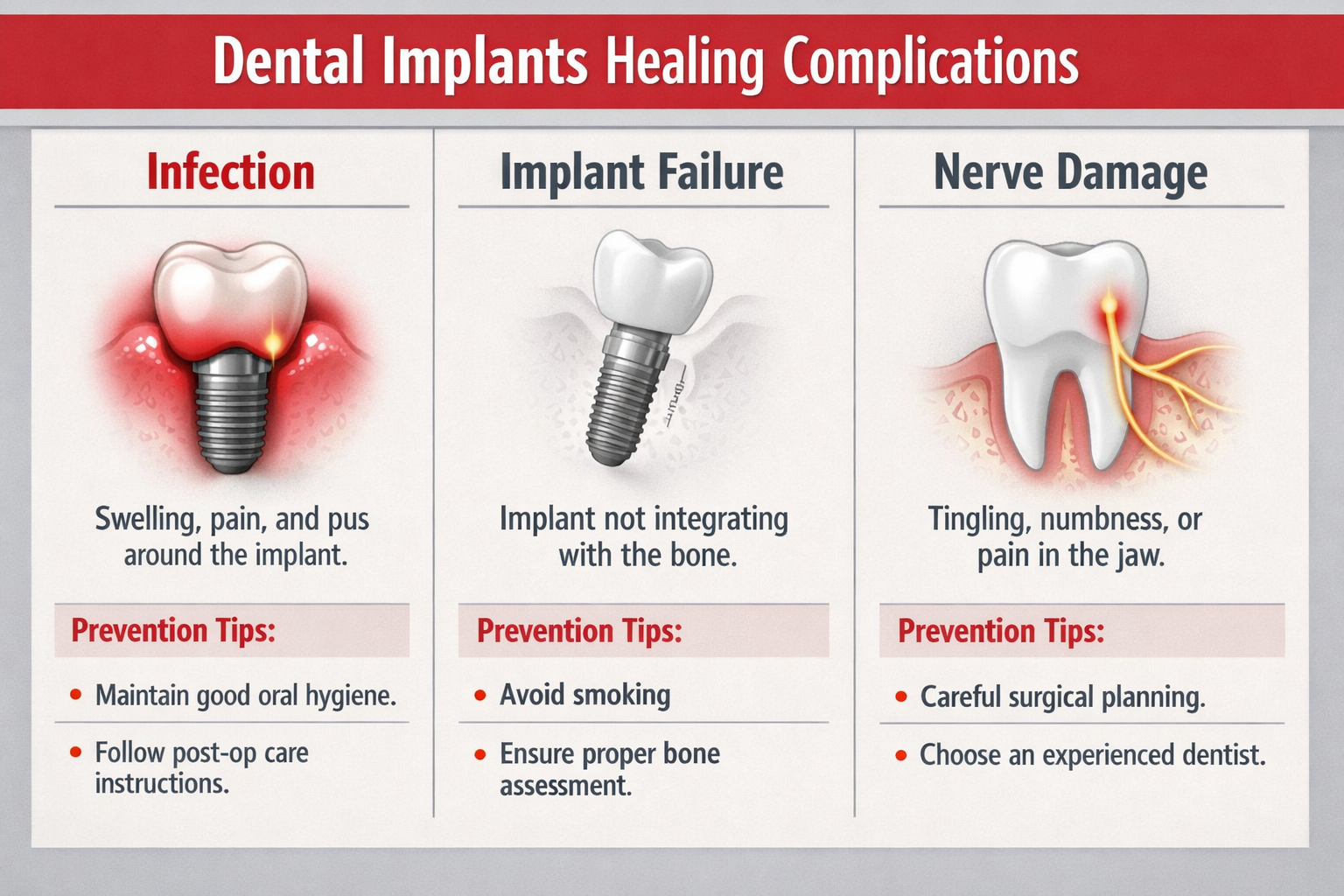
Common Complications and How to Address Them
Though relatively rare, complications can occur. Knowing what to look for can help prevent more serious issues.
- Infection: This is one of the most common complications. Symptoms include increased pain, persistent swelling, redness, warmth, pus discharge, or fever.
- Action: Contact your dentist immediately. Infections often require antibiotics and potentially local irrigation.
- Implant Failure: This occurs when osseointegration does not happen or the implant becomes loose after initial integration. Symptoms include pain, persistent throbbing, swelling, or the implant feeling loose.
- Action: Your dentist will evaluate the implant. Sometimes, removal and re-implantation (possibly with a bone graft) are necessary after the area has healed.
- Nerve Damage: Though uncommon, this can happen if the implant is placed too close to a nerve. Symptoms include numbness, tingling, or pain in the lips, tongue, gums, or chin.
- Action: Report any persistent numbness or unusual sensations to your dentist immediately. Depending on the severity, the implant may need adjustment or removal.
- Sinus Issues (for upper jaw implants): If implants are placed in the upper jaw, they can sometimes penetrate the sinus cavity, leading to sinusitis.
- Action: A bone graft (specifically a sinus lift) is often performed to prevent this, but if symptoms like congestion, pain, or discharge occur, consult your dentist.
When to Contact Your Dentist:
- Severe or worsening pain that isn’t relieved by medication.
- Persistent or increasing swelling after the first 72 hours.
- Excessive bleeding that doesn’t stop with pressure.
- Signs of infection (pus, fever, spreading redness).
- Numbness or tingling that doesn’t resolve.
- If the implant feels loose or shifts.
Factors Influencing Healing and Success
Several factors can impact the speed and success of your dental implants healing journey:
- Oral Hygiene: Meticulous cleaning around the surgical site is paramount. Food debris and bacteria can lead to infection.
- Smoking: As mentioned, smoking is a major risk factor for implant failure. It constricts blood vessels, reducing blood flow to the healing area.
- Underlying Health Conditions: Conditions like uncontrolled diabetes, autoimmune disorders, or certain medications (e.g., bisphosphonates) can impair bone healing. Always provide your dentist with a complete medical history.
- Bone Density and Quality: Adequate, healthy bone is essential for stable osseointegration. If you have experienced 90 percent bone loss in teeth, bone grafting may be necessary.
- Diet: Proper nutrition supports overall healing. A balanced diet rich in vitamins and minerals is beneficial.
- Trauma: Any direct trauma to the implant site during healing can disrupt osseointegration and lead to failure. Be cautious with eating and physical activities.
“A proactive approach and open communication with your dental professional are your strongest allies throughout the dental implants healing process.”
Essential Aftercare and Long-Term Maintenance for Dental Implants
Achieving successful dental implants healing is only the first part of ensuring a lifetime of healthy, functional implants. Diligent aftercare and consistent long-term maintenance are absolutely vital for their longevity and to prevent future complications.
Post-Healing Care: What to Do Once the Implant is Integrated
Once osseointegration is complete and your final crown or prosthesis is attached, your dental implant functions much like a natural tooth. However, it still requires specific care.
- Maintain Excellent Oral Hygiene: This is non-negotiable. Brush at least twice a day with a soft-bristle toothbrush and floss daily. Special floss designed for implants or a water flosser can be particularly effective at cleaning around the implant and crown. Our guide on best dental implant aftercare products can provide excellent recommendations.
- Regular Dental Check-ups: Visit your dentist for regular check-ups and professional cleanings, typically every six months. Your dentist and hygienist will specifically check your implants for any signs of issues and use specialized tools to clean around them without damaging the implant surface or gum tissue.
- Avoid Hard, Sticky Foods: While implants are strong, avoid excessively hard foods (e.g., ice, hard candy) or sticky items that could potentially damage the crown or place undue stress on the implant.
- Address Bruxism (Teeth Grinding): If you grind or clench your teeth (bruxism), your dentist may recommend a nightguard. Bruxism can put excessive force on implants, leading to complications or premature wear.
Recognizing and Preventing Peri-Implantitis
Just like natural teeth can get gum disease (periodontitis), dental implants can develop a similar condition called peri-implantitis. This is an inflammatory disease affecting the soft tissues and bone surrounding a dental implant, which can lead to bone loss and ultimately implant failure if left untreated.
Symptoms of Peri-Implantitis:
- Red, swollen, or bleeding gums around the implant.
- Pus discharge from around the implant.
- Deepening pockets around the implant (measured by your dentist).
- Receding gums around the implant, exposing the metal.
- Pain or tenderness (though often painless until advanced).
- The implant feeling loose.
Prevention is Key:
The best way to prevent peri-implantitis is through exceptional daily oral hygiene and regular professional cleanings. If caught early, it can often be managed with specialized cleaning and antibiotic treatments. However, advanced cases may require surgical intervention.
The Importance of a Specialist Team
Your dental implant journey, from initial consultation to long-term care, benefits immensely from a specialized and experienced team. Professionals who focus on dental implants in Dallas, TX understand the nuances of the healing process and the critical role of comprehensive aftercare. This includes not just the surgeon, but also the restorative dentist who places the crown, and the hygienist trained in implant maintenance.
Proactive Care Checklist:
- ✅ Brush twice daily with a soft brush.
- ✅ Floss daily with appropriate tools.
- ✅ Use recommended mouthwash (non-alcoholic, implant-safe).
- ✅ Attend all follow-up appointments.
- ✅ Schedule regular professional cleanings.
- ✅ Report any changes or concerns immediately.
- ✅ Avoid tobacco products.
- ✅ Manage underlying health conditions effectively.
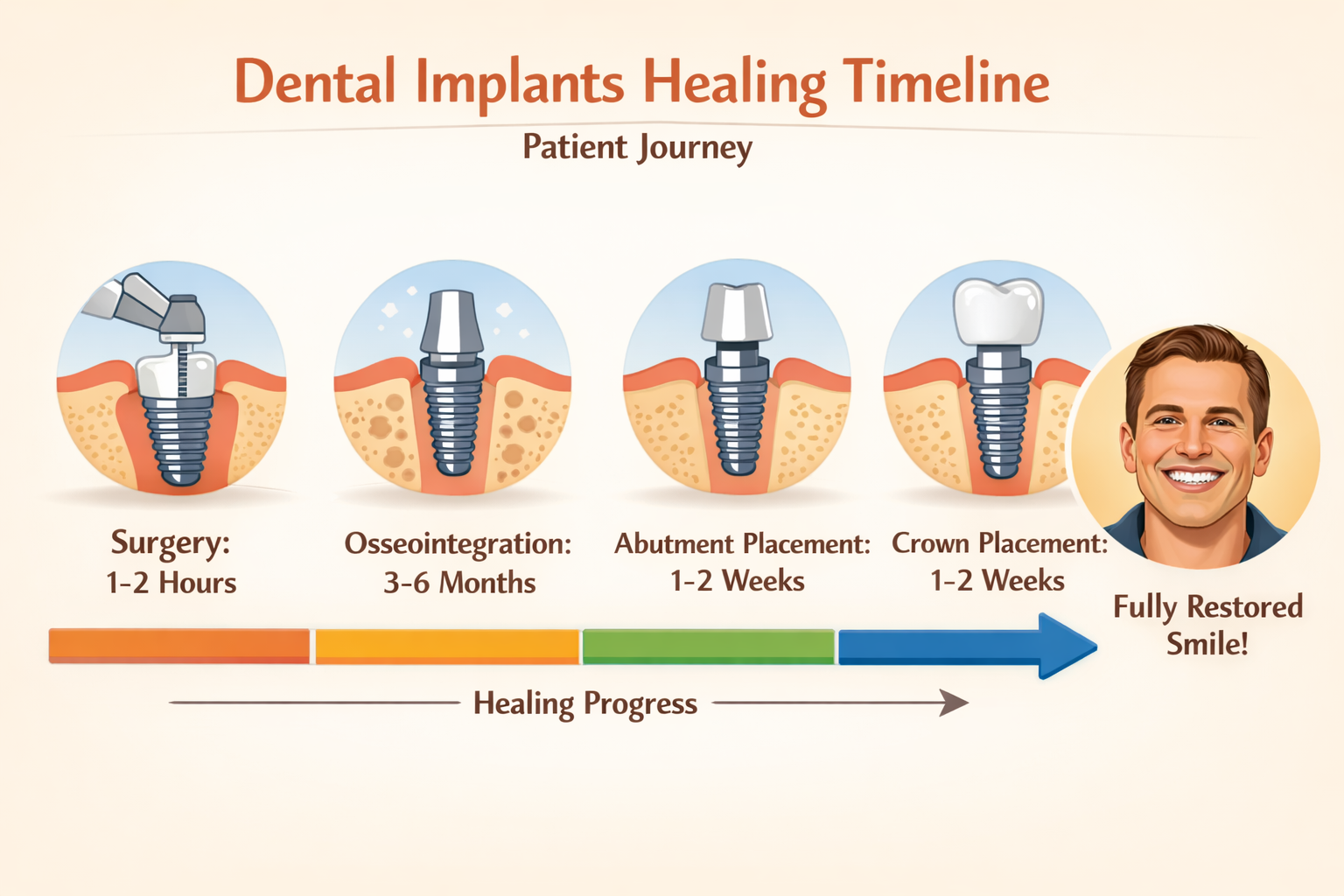
Dental Implants Healing Timeline: A General Overview

Understanding the general dental implants healing timeline can help manage expectations and provide a roadmap for your journey. Keep in mind that individual experiences can vary significantly.
Phase 1: Initial Healing (1-2 Weeks)
- Day 1-3: Bleeding, swelling, and mild to moderate pain are common. Strict adherence to soft diet and pain management.
- Day 4-7: Swelling and pain begin to subside. Introduction of gentle saltwater rinses or prescribed mouthwash. Continued soft diet. Sutures (if present) may dissolve or be removed.
- Week 2: Most initial discomfort should be gone. Gradual return to a slightly less restrictive diet, but still avoiding chewing on the implant site.
Phase 2: Osseointegration (3-6 Months, potentially longer with bone grafts)
- Months 1-2: Bone cells begin to grow onto the implant surface. The implant is stable but not yet fully integrated. Still avoiding direct chewing on the implant.
- Months 3-6: Osseointegration progresses significantly. The jawbone fuses directly with the implant. Your dentist will typically confirm successful integration with X-rays before proceeding.
- Note: If a bone graft was required, this phase could extend to 6-9 months or even a year before full stability is achieved. For example, a bone graft recovery dental implant process adds significant time.
Phase 3: Abutment Placement and Final Restoration (2-4 Weeks)
- Abutment Placement: After osseointegration, a minor procedure to expose the implant and attach the abutment. This typically involves local anesthesia and a short healing period of 1-2 weeks. You can learn more about this step in our complete guide to the dental implant abutment procedure.
- Crown/Prosthesis Placement: Once the gums around the abutment have healed, impressions are taken to create your custom crown, bridge, or denture. This final restoration is then permanently attached, completing your new smile. This phase often takes 1-2 weeks for fabrication and placement.
Phase 4: Long-Term Maintenance (Ongoing)
- Regular Check-ups and Cleanings: Essential every 6 months (or as advised by your dentist).
- Daily Oral Hygiene: Consistent brushing and flossing are paramount for the life of your implants.
- Vigilance: Report any discomfort or changes around your implants to your dentist promptly.
This comprehensive journey ensures that your dental implants become a permanent and comfortable part of your oral health. While it might seem like a long process, the vast majority of patients find the results — a fully restored, confident smile — well worth the investment in time and care. For a deeper dive into the entire process, consider reading our complete dental implant recovery timeline.
Conclusion: Embracing a Successful Dental Implant Future in 2026
The journey through dental implants healing is a testament to modern dentistry’s ability to restore not just teeth, but confidence and quality of life. From the initial delicate days post-surgery, through the crucial months of osseointegration, and into the lifelong commitment of maintenance, each step plays a vital role in the success and longevity of your dental implants. By understanding this process, adhering to aftercare instructions, and maintaining open communication with your dental team, you are actively participating in securing a healthy and brilliant smile for years to come.
Remember that while the general timelines and expectations provided here offer a valuable guide, your personal healing journey is unique. Factors such as your overall health, bone quality, and adherence to post-operative care will all influence your individual experience.
Actionable Next Steps:
- Strictly Follow Instructions: Always follow the specific post-operative care instructions provided by your dental professional.
- Maintain Oral Hygiene: Develop and stick to an impeccable daily oral hygiene routine, tailored for implants.
- Attend All Appointments: Do not skip any follow-up appointments or regular dental check-ups. These are critical for monitoring healing and long-term health.
- Communicate Concerns: If you experience any unusual pain, swelling, or have concerns at any stage of your healing, contact your dentist immediately.
- Choose an Experienced Team: Partner with a reputable and experienced dental implant specialist, like those you can find by visiting https://dentalimplantsdallastx.com/.
By committing to these steps, you are not just healing an implant; you are investing in a future of improved oral function, aesthetics, and overall well-being. Here’s to a successful healing process and a radiant smile in 2026 and beyond!
References
[1] Albrektsson, T., & Sennerby, L. (1990). State of the art in oral implants. Journal of Clinical Periodontology, 17(7), 467-471.
[2] Esposito, M., Hirsch, J. M., Lekholm, U., & Thomsen, R. (1998). Biological factors contributing to failures of osseointegrated oral implants.(I). Success criteria and epidemiology. European Journal of Oral Sciences, 106(5), 527-551.
[3] Renvert, S., & Quirynen, M. (2019). Risk factors for dental implant failure and peri-implantitis. Periodontology 2000, 79(1), 1-2.
Dental Implant Healing Timeline Calculator
Estimate your dental implants healing journey based on common factors. Remember, this is an estimate; consult your dentist for personalized advice.
Your Estimated Healing Milestones (2026)
Based on your input, here’s an estimated timeline for your dental implant healing:
Important Note: This calculator provides a general estimate. Individual healing varies. Always follow your dentist’s specific instructions and consult them for your precise timeline and care plan. The current year for these estimates is 2026.

Leave a Reply
Share your thoughts or ask a question about dental implants. Your email address will not be published.