When I first learned that dental implants could fail and require removal, I was shocked. After all, these titanium posts are supposed to be permanent solutions for missing teeth. Yet here’s the reality: while dental implants have a high success rate of 95-98%, failures do occur, and when they do, understanding your options for dental implant removal becomes crucial for your oral health and future treatment success.
Key Takeaways
- Dental implant removal is necessary when implants fail due to infection, mechanical issues, or poor integration with surrounding bone
- Multiple removal techniques are available, from simple unscrewing to complex surgical procedures, depending on the implant’s condition
- Future implant placement is often possible after proper healing and bone grafting at the removal site
- Early detection of implant problems significantly improves treatment outcomes and reduces complications
- Professional expertise is essential – choosing an experienced dental implant specialist ensures safe and effective removal procedures
Understanding Dental Implant Failure and the Need for Removal
Dental implant failure occurs when the titanium implant cannot properly integrate with your jawbone or when complications arise after successful integration. While the survival rate of implants placed in optimal conditions exceeds 95%, certain factors can lead to implant failure requiring removal.
Early implant failure typically happens within the first few months after implant placement, usually due to:
- Poor osseointegration (bone-to-implant integration)
- Infection at the implant site
- Inadequate bone quality or quantity
- Surgical complications
Late implant failure can occur years after successful integration, often caused by:
- Peri-implantitis (infection around the implant)
- Mechanical complications like implant fracture
- Excessive bite forces
- Poor oral hygiene leading to bone loss
Understanding these failure patterns helps both patients and dental professionals recognize when removal of dental implants becomes necessary.
Common Reasons for Dental Implant Removal
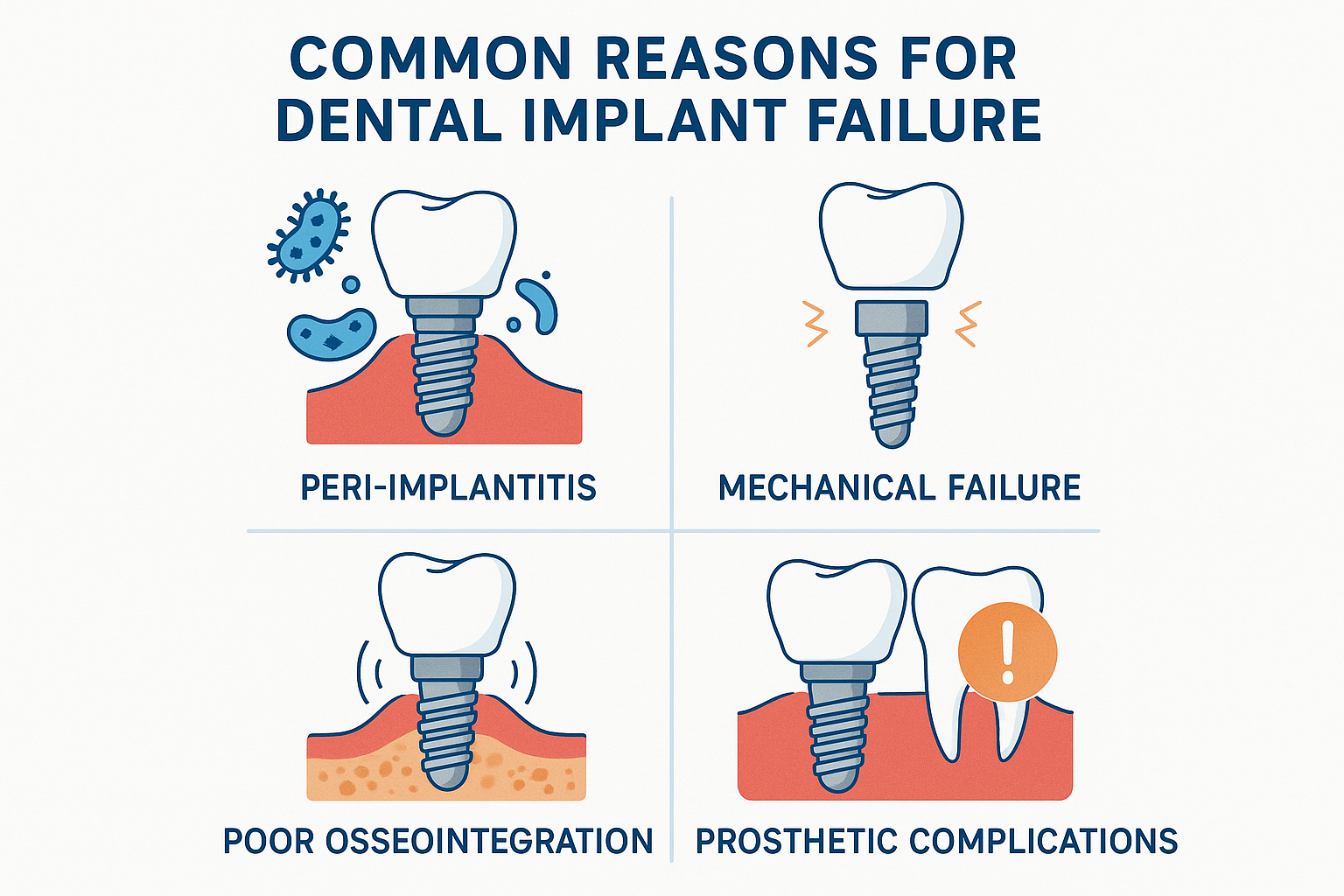
🦠 Peri-Implantitis and Infection
Peri-implantitis is the leading cause requiring removal of failed dental implants. This bacterial infection affects the tissues surrounding the implant, causing inflammation and progressive bone loss around the implant site. When conservative treatments fail to control the infection, removing a failed implant becomes the only viable option to preserve remaining bone and prevent further complications.
🔧 Mechanical Complications
Implant fracture represents a serious mechanical complication that often necessitates implant removal. The implant body or implant connection can break due to:
- Manufacturing defects
- Excessive occlusal forces
- Metal fatigue over time
- Improper implant placement
When an implant fracture occurs, specialized implant removal techniques are required to extract the broken pieces without damaging the surrounding bone.
📉 Poor Osseointegration
Sometimes, the dental implant fails to integrate properly with the jawbone, remaining loose or mobile. This lack of osseointegration means the implant cannot function as intended, and removal is required before attempting a new implant placement.
🏗️ Prosthetic Complications
Certain prosthetic complications may require implant removal, particularly when:
- The implant position prevents proper restoration
- Multiple implant failures affect the overall treatment plan
- Aesthetic concerns cannot be resolved with the current implant
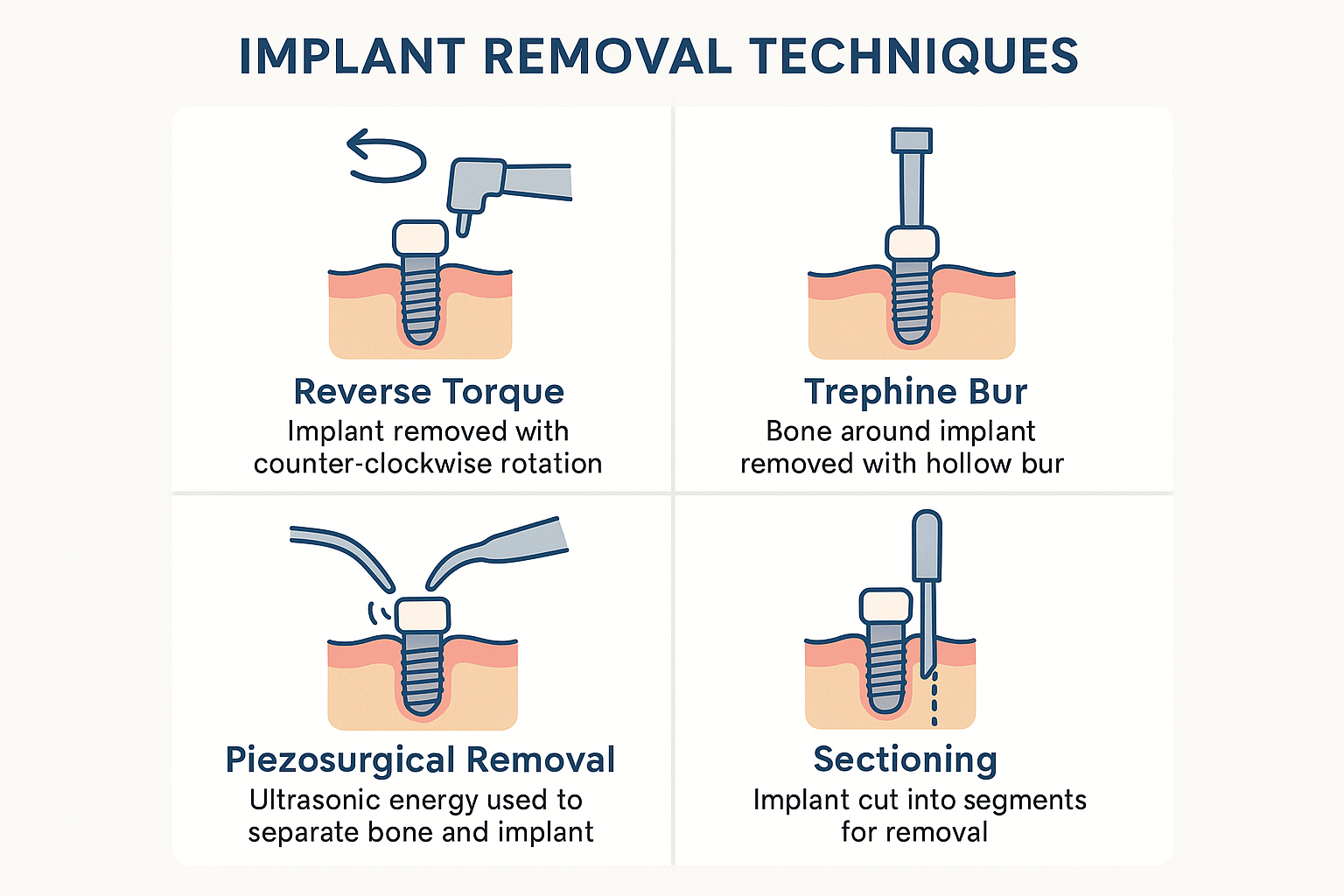
Implant Removal Techniques: From Simple to Complex
The method for implant removal depends on several factors, including the degree of osseointegration, implant condition, and surrounding bone quality. Here are the primary implant removal techniques used by dental professionals:
Reverse Torque Technique
For implants with minimal osseointegration, the reverse torque method involves carefully unscrewing the implant using specialized instruments. This conservative implant removal technique preserves the maximum amount of surrounding bone and is ideal when:
- The implant is mobile or loose
- Osseointegration is poor
- No implant fracture has occurred
Trephine Bur Technique
When implants are well-integrated, a trephine bur can be used to carefully cut around the implant body, breaking the bone-to-implant connection. This technique for the removal of osseointegrated dental implants requires:
- Precise surgical planning
- Careful depth control
- Adequate irrigation to prevent overheating
Piezosurgical Removal
The piezosurgical removal of fractured implants represents an advanced technique using ultrasonic vibrations to selectively cut bone while preserving soft tissues. This method is particularly effective for:
- Removing broken implant pieces
- Minimizing trauma to surrounding tissues
- Preserving bone for future implant placement
Sectioning Technique
For complex cases involving implant fracture, the sectioning technique involves cutting the implant into smaller pieces for easier removal. This method requires:
- High-speed cutting instruments
- Careful planning to avoid damage to adjacent structures
- Expertise in managing fractured implant components
The Dental Implant Removal Process: What to Expect
Understanding the removal process helps patients prepare mentally and physically for the procedure. Here’s what typically happens during dental implant removal:
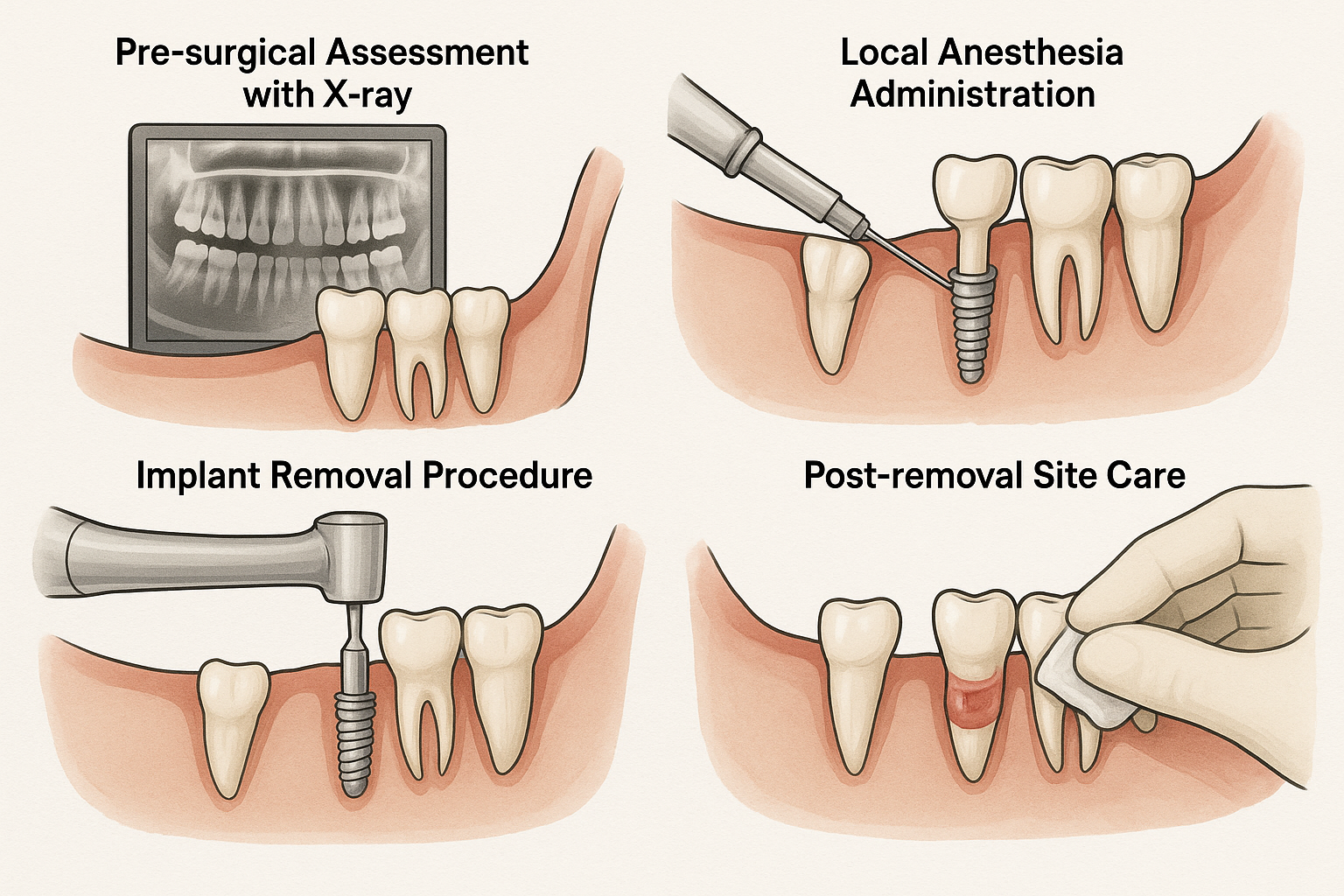
Pre-Surgical Assessment
Before any removal procedure, your dentist will conduct a thorough evaluation including:
- 3D imaging to assess bone quality and implant position
- Medical history review to identify risk factors
- Treatment planning to determine the best removal approach
- Discussion of future options for tooth replacement
The Removal Procedure
The actual removal surgery varies based on the chosen technique:
- Local anesthesia administration for patient comfort
- Soft tissue management to access the implant
- Implant removal using the selected technique
- Site debridement to remove infected or damaged tissue
- Bone grafting if needed to preserve the removal site
- Suturing and post-operative instructions
Immediate Post-Removal Care
Following implant removal, proper care is essential for healing:
- Pain management with prescribed medications
- Swelling control using ice packs
- Oral hygiene modifications to protect the healing site
- Diet restrictions to promote optimal healing
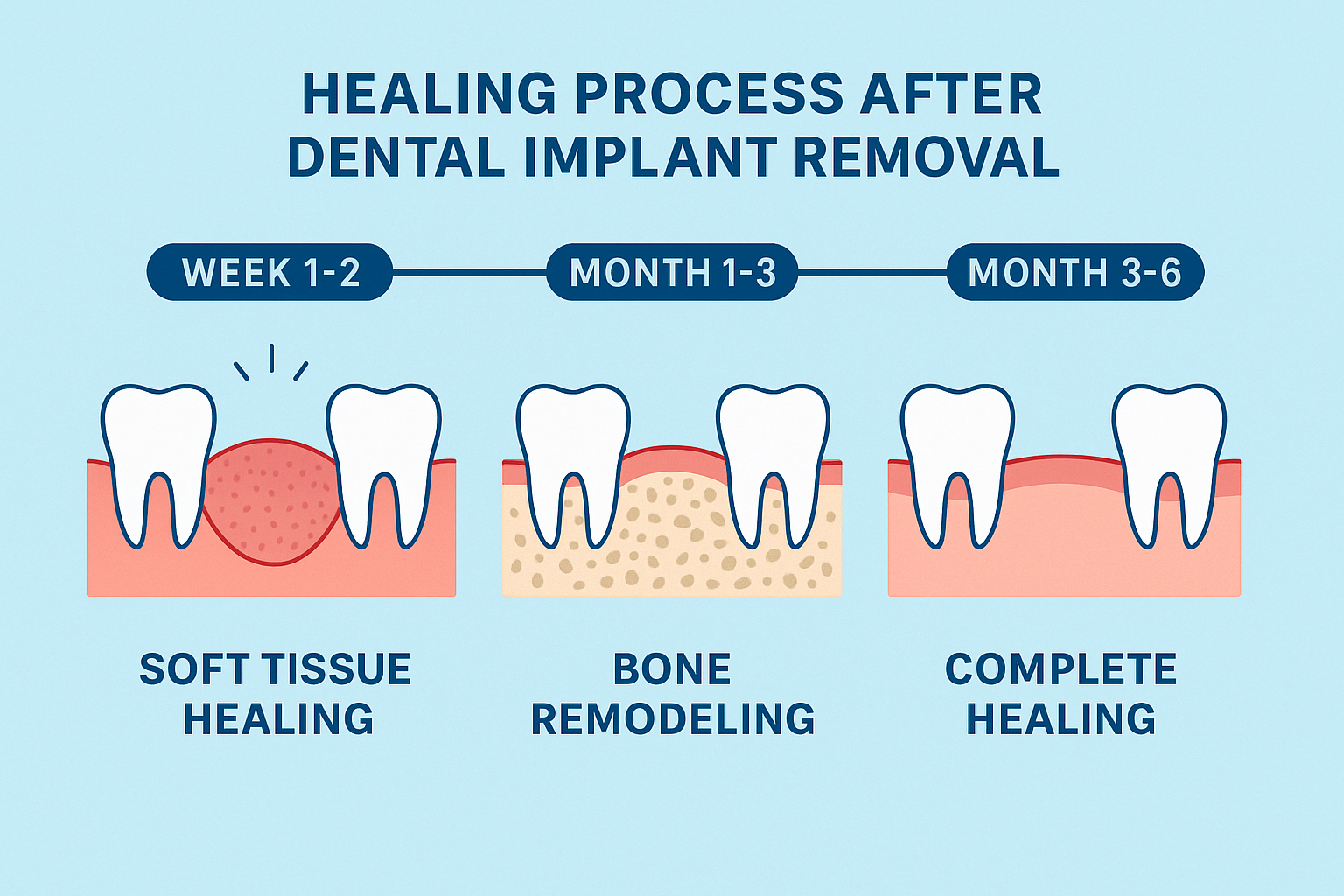
Recovery and Healing After Implant Removal
The healing process following dental implant removal typically takes 3-6 months, depending on various factors including the removal technique used and whether bone grafting was performed.
Timeline for Healing
Week 1-2: Initial soft tissue healing
- Swelling and discomfort peak and begin to subside
- Sutures may be removed
- Soft diet recommended
Month 1-3: Bone remodeling begins
- Soft tissue healing completes
- Early bone formation at the removal site
- Gradual return to normal diet
Month 3-6: Complete bone healing
- Mature bone formation
- Site ready for evaluation for new implant placement
- Full function restoration possible
Factors Affecting Recovery
Several factors influence healing after implant removal:
- Patient age and health status
- Smoking habits (significantly delays healing)
- Bone quality at the removal site
- Presence of infection prior to removal
- Compliance with post-operative instructions
Can You Get a New Dental Implant After Removal?
One of the most common questions patients ask is whether a new dental implant can be placed after removal. The answer is often yes, but several factors determine the success of implant replacement:
Site Assessment for New Implant
Before placing a new implant, your dentist will evaluate:
- Bone volume and quality at the removal site
- Soft tissue health and thickness
- Reason for previous failure and how to prevent recurrence
- Patient factors that may affect success
Bone Grafting Requirements
In many cases, bone grafting is necessary before placing a new implant. The bone graft helps:
- Restore bone volume lost during the failure process
- Improve bone quality for better osseointegration
- Create optimal conditions for implant success
Timeline for New Implant Placement
The timing for a new dental implant depends on:
- Healing progress at the removal site
- Bone graft integration (if performed)
- Resolution of infection or other complications
- Patient readiness for additional treatment
Most patients can receive a new implant 3-6 months after removal, though complex cases may require longer healing periods.
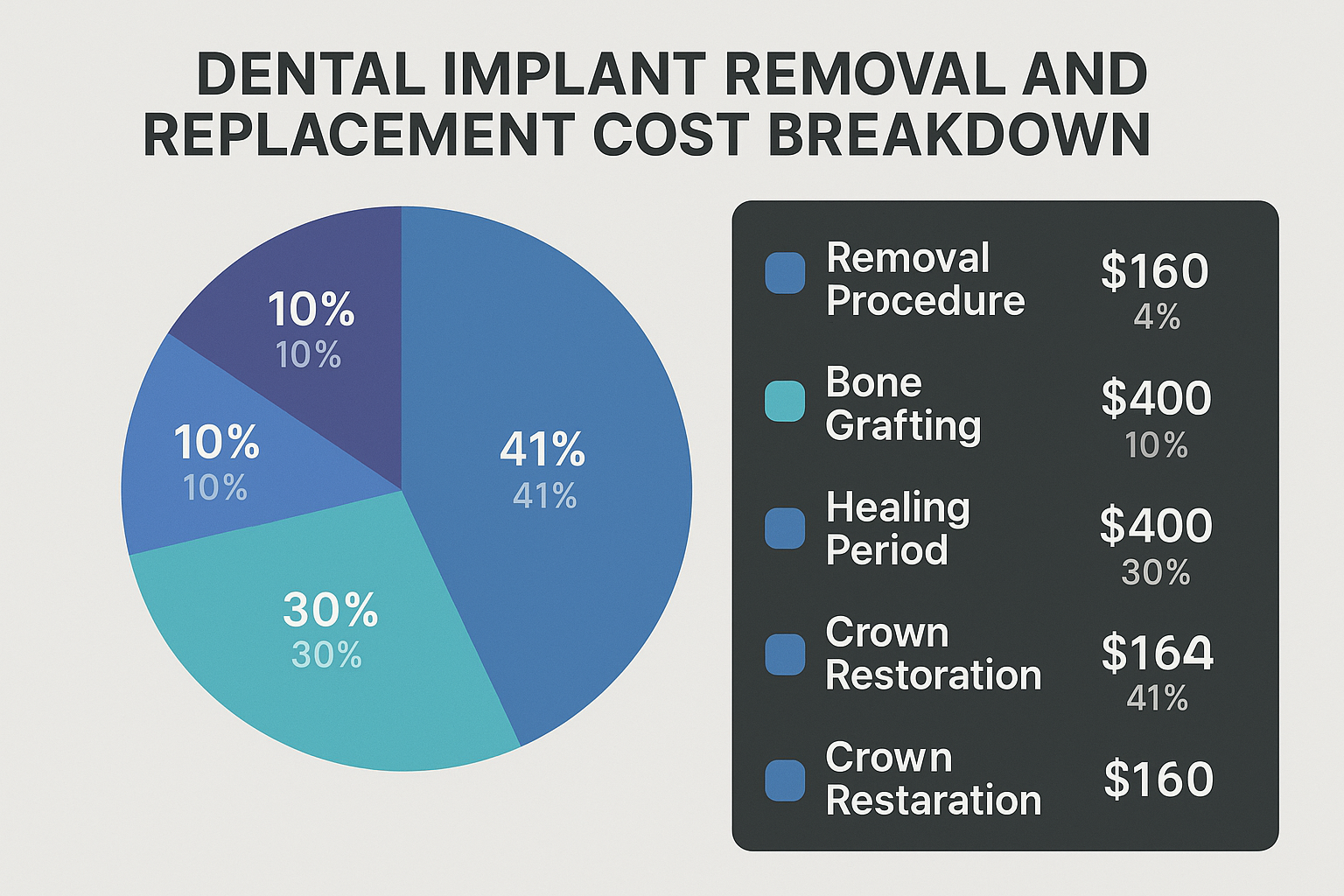
Cost Considerations for Dental Implant Removal
The cost of dental implant removal varies significantly based on the complexity of the procedure and additional treatments required. Understanding these factors affecting implant cost helps patients plan financially for treatment.
Factors Influencing Removal Costs
- Complexity of removal (simple vs. surgical)
- Need for bone grafting at the removal site
- Geographic location and practice overhead
- Specialist involvement (oral surgeon vs. general dentist)
- Additional procedures required
Insurance Coverage
Many dental insurance plans provide coverage for medically necessary implant removal, particularly when:
- Infection poses a health risk
- Pain significantly impacts quality of life
- The implant interferes with other necessary treatments
Check with your insurance provider about coverage for both removal and replacement procedures.
Financial Planning Options
For patients concerned about costs, several options are available:
- Payment plans offered by dental practices
- Dental financing through third-party companies
- Consultation with multiple providers for cost comparison
- Phased treatment to spread costs over time
Consider exploring affordable dental implants and payment plans for implants to make treatment more manageable.
🦷 Dental Implant Failure Risk Assessment
Answer these questions to assess your implant’s condition and determine if removal consultation is needed
Recommended Actions:
Prevention: Avoiding Future Implant Failures
While some implant failures are unavoidable, many can be prevented through proper care and risk management. Understanding how to protect your investment in dental implants is essential for long-term success.
Maintaining Optimal Oral Hygiene
The foundation of implant longevity lies in excellent oral hygiene:
Daily Care Routine:
- Brush twice daily with a soft-bristled toothbrush
- Use fluoride toothpaste to protect surrounding teeth
- Floss daily around the implant with specialized floss
- Consider water flossing for enhanced cleaning
Professional Maintenance:
- Regular dental cleanings every 3-6 months
- Professional monitoring of implant health
- Early detection of potential problems
- Prompt treatment of any complications
Risk Factor Management
Controlling modifiable risk factors significantly reduces the chance of implant failure:
Smoking Cessation: Smoking is one of the strongest predictors of implant failure. Quitting smoking before and after implant treatment dramatically improves success rates.
Diabetes Management: Well-controlled diabetes doesn’t prevent implant success, but poor glucose control increases failure risk.
Bite Force Management: Using a night guard if you grind your teeth protects implants from excessive forces.
Regular Professional Monitoring
Routine follow-up care allows early detection of problems:
- Annual X-rays to monitor bone levels
- Clinical examinations to assess soft tissue health
- Bite analysis to ensure proper force distribution
- Patient education about warning signs
Choosing the Right Professional for Implant Removal
The success of dental implant removal depends heavily on the expertise of the treating professional. Choosing a dental implant dentist with specific experience in implant removal is crucial for optimal outcomes.
Qualifications to Look For
When selecting a professional for implant removal, consider:
Specialized Training:
- Advanced education in implant dentistry
- Specific training in implant removal techniques
- Experience with complex cases
- Continuing education in latest techniques
Technology and Equipment:
- 3D imaging capabilities for precise planning
- Specialized removal instruments
- Piezoelectric surgery equipment
- Proper sterilization and safety protocols
Track Record:
- Experience with similar cases
- Before and after case examples
- Patient testimonials and reviews
- Complication management experience
Questions to Ask Your Dentist
Before proceeding with implant removal, ask these important questions:
- “What technique do you recommend for my specific case?”
- “How many similar procedures have you performed?”
- “What are the risks and potential complications?”
- “Can a new implant be placed in the future?”
- “What will the recovery process involve?”
- “What are my options for temporary tooth replacement?”
Alternative Treatment Options
When dental implant removal becomes necessary, patients have several options for replacing the missing tooth:
Immediate Replacement Options
Removable Partial Denture: A temporary solution that can be worn immediately after implant removal while the site heals.
Temporary Bridge: In some cases, a temporary bridge can restore function and aesthetics during the healing period.
Long-term Replacement Solutions
New Dental Implant: After proper healing and any necessary bone grafting, a new implant can often be placed with excellent success rates.
Fixed Bridge: A traditional bridge using adjacent teeth as anchors can provide a permanent solution when implant replacement isn’t possible.
Removable Prosthetics: Modern removable appliances offer improved comfort and function compared to traditional dentures.
Factors Influencing Treatment Choice
The best replacement option depends on:
- Bone quality at the removal site
- Adjacent tooth condition
- Patient preferences and lifestyle
- Financial considerations
- Timeline requirements
Long-term Outlook and Success Rates
The prognosis following dental implant removal is generally positive, especially when proper protocols are followed and adequate healing time is allowed.
Success Rates for Replacement Implants
Research shows that implants placed in previously failed sites can achieve success rates comparable to primary implants when:
- Adequate healing time is allowed (3-6 months minimum)
- Proper site preparation is performed
- Risk factors are addressed
- Appropriate technique is used
Studies indicate that implants placed in previously failed sites achieve success rates of 85-95% when proper protocols are followed.
Factors Affecting Long-term Success
Patient Factors:
- Age and overall health
- Smoking status
- Oral hygiene compliance
- Systemic diseases
Site Factors:
- Bone quality and quantity
- Soft tissue health
- Previous infection resolution
- Adequate healing time
Technical Factors:
- Proper implant selection
- Optimal placement technique
- Appropriate loading protocols
- Quality of prosthetic restoration
Managing Costs and Insurance Considerations
Understanding the financial aspects of dental implant removal and replacement helps patients make informed decisions about their treatment.
Typical Cost Ranges
Simple Implant Removal: $500-$1,500
- Minimal surgical intervention required
- Local anesthesia sufficient
- Outpatient procedure
Complex Surgical Removal: $1,500-$4,000
- Extensive surgical access needed
- Possible sedation required
- Additional procedures like bone grafting
Total Treatment Cost (including replacement): $3,000-$8,000
- Varies by geographic location
- Depends on complexity of case
- Includes all phases of treatment
For more information about managing costs, explore options for low-cost dental implants and affordable implants.
Insurance Coverage Strategies
Medical Necessity Documentation:
- Clear documentation of implant failure
- Evidence that removal is medically necessary
- Detailed treatment plan from qualified professional
Pre-authorization Process:
- Submit treatment plan before beginning
- Include supporting radiographs and clinical photos
- Provide detailed cost breakdown
Appeal Process:
- Understand your insurance company’s appeal procedures
- Gather additional supporting documentation if needed
- Consider involving your dentist in the appeal process
Financial Planning Tips
Treatment Phasing:
- Separate removal and replacement into different benefit years
- Maximize annual insurance benefits
- Allow adequate healing time between phases
Payment Options:
- Dental practice payment plans
- Third-party financing companies
- Health savings accounts (HSA) or flexible spending accounts (FSA)
- Personal loans or credit options
Conclusion
Dental implant removal, while not ideal, is sometimes necessary to preserve your oral health and create opportunities for successful future treatment. Understanding the reasons for implant failure, available removal techniques, and your options for replacement empowers you to make informed decisions about your dental care.
The key to successful outcomes lies in:
- Early recognition of implant problems
- Prompt professional consultation when issues arise
- Choosing experienced professionals for removal procedures
- Following proper healing protocols before replacement
- Addressing risk factors to prevent future failures
Remember that implant failure doesn’t mean you can’t have successful implant treatment in the future. With proper removal techniques, adequate healing time, and appropriate risk factor management, many patients go on to enjoy successful implant replacement.
If you’re experiencing any signs of implant problems, don’t wait. Early intervention often provides the best outcomes and may even save a failing implant. Contact a qualified dental professional to discuss your symptoms and explore your treatment options.
Your oral health is worth the investment in proper care, and with the right approach, you can maintain a healthy, functional smile for years to come.

Leave a Reply
Share your thoughts or ask a question about dental implants. Your email address will not be published.