Experiencing dental implant pressure pain when biting down can be an alarming and uncomfortable sensation, often leading to concern about the success and longevity of your dental investment. While dental implants are renowned for their durability and ability to restore chewing function, any persistent pain, especially under pressure, warrants immediate attention. This article, updated for 2026, aims to thoroughly explore the various reasons behind dental implant pressure pain when biting down, guiding you through potential causes, diagnostic methods, and effective treatment strategies. Our goal is to empower you with the knowledge to understand this specific issue and encourage you to seek professional dental advice promptly.
Key Takeaways
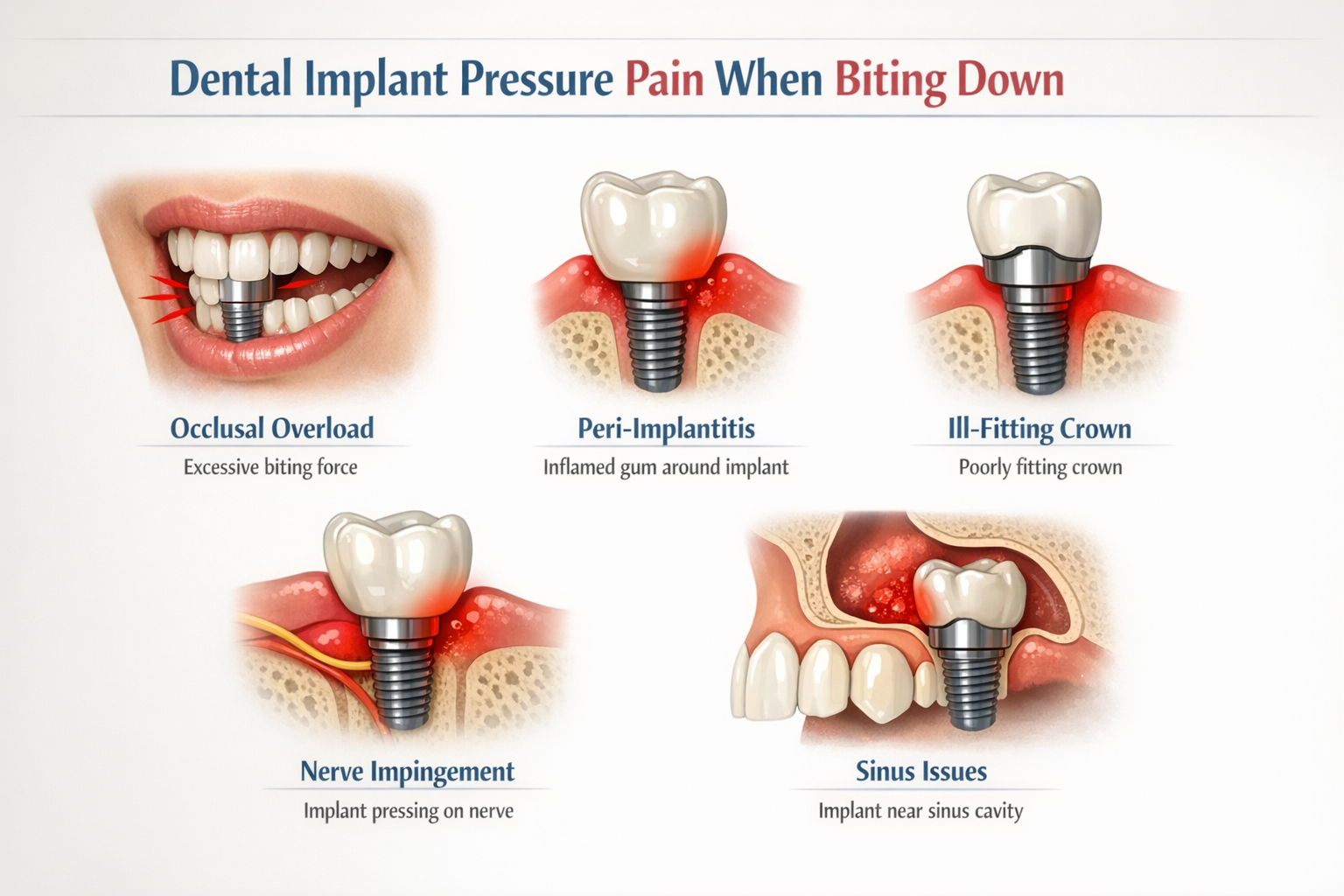
- Diverse Causes: Dental implant pressure pain can stem from various issues, including occlusal overload, peri-implantitis, nerve impingement, or an ill-fitting crown.
- Early Intervention is Crucial: Prompt dental evaluation is essential to accurately diagnose the root cause and prevent more severe complications.
- Diagnostic Tools: Dentists utilize advanced tools like X-rays, CT scans, and occlusal analysis to pinpoint the source of discomfort.
- Tailored Treatment: Treatment options vary widely, from simple occlusal adjustments to antibiotic therapy or surgical intervention, depending on the diagnosis.
- Proactive Care: Maintaining excellent oral hygiene and regular dental check-ups are key to preventing implant-related issues and ensuring long-term success.
Understanding Dental Implant Pressure Pain When Biting Down
Dental implants are sophisticated dental prosthetics designed to replace missing teeth, offering a stable and long-lasting foundation for crowns, bridges, or dentures. They consist of a titanium post surgically placed into the jawbone, an abutment that connects the post to the prosthetic tooth, and the prosthetic tooth itself. The process of osseointegration, where the implant fuses with the jawbone, is critical for their stability and success. When this process is complete, a properly integrated implant should feel as natural and comfortable as a healthy tooth.
However, if you experience dental implant pressure pain when biting down, it signals that something is amiss. Unlike natural teeth, which have a periodontal ligament that provides proprioception (the sense of position and movement), dental implants directly integrate with bone. This means that sensations around an implant can feel different and pain under pressure is a direct indicator of a problem, rather than just sensitivity. It’s important to differentiate between temporary post-surgical discomfort and persistent or new-onset pain after the implant has healed and been put into function. Ignoring this pain can lead to complications that compromise the implant’s integrity and your overall oral health.
The Anatomy of an Implant and Pain Perception
To grasp why you might feel dental implant pressure pain when biting down, it helps to understand the components involved:
- Implant Post (Fixture): The titanium screw surgically placed into the jawbone.
- Abutment: A connector piece that attaches to the implant post and extends through the gum line.
- Prosthetic Crown/Bridge/Denture: The visible part that functions as the tooth.
Pain perception around an implant is primarily due to nerve endings in the surrounding bone, gums, or adjacent teeth. When pressure is applied during biting, any underlying issue can manifest as discomfort or sharp pain. This could range from a minor irritation to a significant infection or mechanical problem.
Common Causes of Dental Implant Pressure Pain When Biting Down
The reasons for experiencing dental implant pressure pain when biting down can be varied, ranging from simple, easily resolvable issues to more complex conditions requiring specialized intervention. Identifying the exact cause is paramount for effective treatment.
1. Occlusal Overload (Bite Problems)
One of the most frequent culprits behind dental implant pressure pain when biting down is occlusal overload, also known as bite problems or malocclusion. This occurs when the forces applied during chewing are not evenly distributed across the implant and surrounding teeth.
- High Spots: If the prosthetic crown on your implant is slightly taller than your natural teeth, it will bear excessive force every time you bite. This “high spot” can put undue pressure on the implant and the surrounding bone, leading to discomfort, inflammation, and even bone loss over time. It’s a common issue, especially soon after the crown is placed or if your bite shifts.
- Bruxism/Clenching: Habitual teeth grinding (bruxism) or clenching, particularly at night, can exert tremendous, sustained forces on dental implants. While implants are strong, chronic overloading can lead to micro-fractures in the bone, inflammation around the implant, or even damage to the implant components themselves. Patients who grind their teeth may require custom night guards to protect their implants and natural teeth.
- Inadequate Osseointegration: Although less common if the implant has been in function for a while, insufficient or failed osseointegration can make an implant less stable and more susceptible to pain under pressure. If the implant hasn’t fully fused with the bone, it might move slightly when subjected to chewing forces, causing pain.
2. Peri-Implantitis
Peri-implantitis is an inflammatory condition affecting the tissues surrounding a dental implant, leading to progressive bone loss around the implant. It’s akin to periodontal disease in natural teeth and is a significant concern for long-term implant success.
- Bacterial Infection: The primary cause of peri-implantitis is bacterial plaque accumulation around the implant. Poor oral hygiene allows bacteria to thrive, creating an infection that damages the gum tissue and eventually the supporting bone.
- Symptoms: Beyond dental implant pressure pain when biting down, symptoms can include redness, swelling, bleeding gums around the implant, pus discharge, and a noticeable increase in pocket depth around the implant. In advanced stages, the implant may become mobile. Regular cleanings and vigilant home care are critical for prevention. You can learn more about proper care at dentalimplantsdallastx.com/best-dental-implant-aftercare-products/.
3. Nerve Impingement or Damage
While rare, nerve issues can cause significant dental implant pressure pain when biting down, especially if the implant was placed in close proximity to a major nerve pathway.
- Inferior Alveolar Nerve: In the lower jaw, the inferior alveolar nerve runs through the bone, providing sensation to the teeth, gums, and lower lip. If an implant is placed too close to or directly impinges upon this nerve, it can cause pain, numbness, tingling, or an electric-shock sensation, particularly when pressure is applied.
- Mental Nerve: The mental nerve is a branch of the inferior alveolar nerve that exits the jawbone near the chin. Impingement here can cause similar symptoms in the lip and chin area.
- Symptoms: Besides pain with biting, patients might experience persistent numbness, tingling (paresthesia), or an altered sensation in the lip, chin, or tongue. This usually occurs immediately or shortly after surgery but can sometimes manifest later if there’s progressive bone remodeling.
4. Ill-Fitting or Damaged Prosthetic Components
The crown, abutment, or even the implant itself can be the source of discomfort if compromised.
- Loose or Damaged Crown/Abutment: If the screw holding the crown to the abutment, or the abutment to the implant, becomes loose or fractured, it can create instability. This instability will cause pain or discomfort when biting down, as the components shift under pressure. You might also notice a clicking noise or a feeling of looseness. Understanding the abutment placement process can help in understanding this connection.
- Fractured Implant: Although titanium implants are incredibly strong, a severe fracture of the implant post itself can occur due to extreme forces or manufacturing defects. This is a serious complication and typically results in significant pain and implant mobility.
- Cement Residue: Sometimes, excess dental cement used to bond the crown to the abutment can be left under the gum line. This residue can irritate the surrounding tissues, leading to inflammation and discomfort, mimicking peri-implantitis.
5. Sinus Issues (for Upper Jaw Implants)
Implants placed in the upper jaw, particularly in the molar and premolar regions, are in close proximity to the maxillary sinuses.
- Sinus Perforation/Infection: If an implant penetrates the sinus cavity during placement or if a sinus lift procedure leads to complications, it can cause sinus inflammation or infection (sinusitis). This can manifest as pressure pain that worsens when biting down, especially on the affected side, and may be accompanied by congestion or post-nasal drip.
- Insufficient Bone Graft Healing: If a bone graft for dental implants was performed in the sinus area, incomplete or complicated healing could also be a source of discomfort.
6. Adjacent Tooth Problems
Sometimes, the pain you perceive around an implant might actually be originating from a neighboring natural tooth.
- Decay or Abscess: A deep cavity or an infection in an adjacent tooth can radiate pain that feels like it’s coming from the implant.
- Periodontal Disease: Gum disease in a tooth next to the implant can also cause inflammation and tenderness that might be misattributed to the implant.
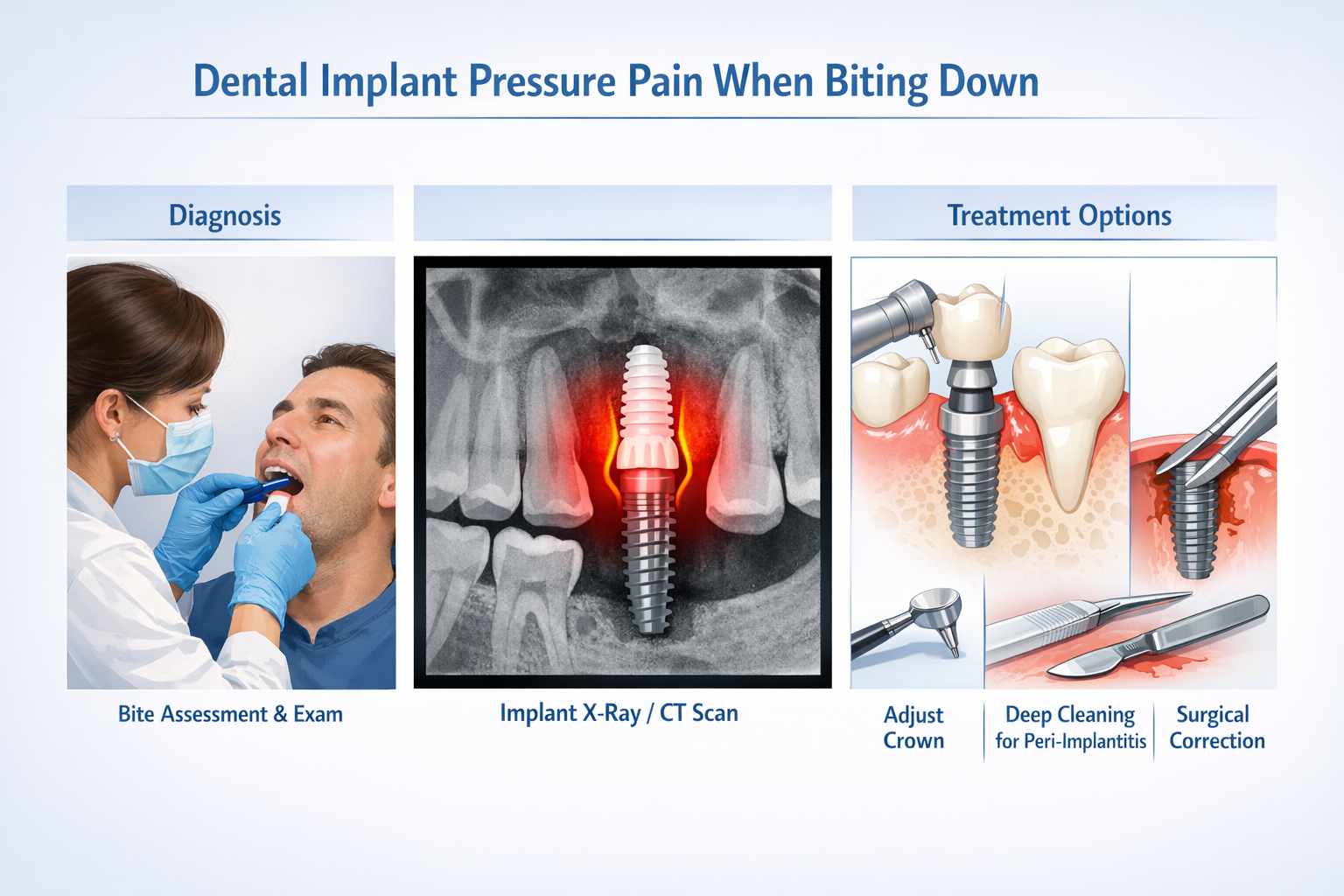
Diagnosing Dental Implant Pressure Pain When Biting Down
When you present with dental implant pressure pain when biting down, your dentist will undertake a systematic diagnostic process to identify the underlying cause. This typically involves a combination of clinical examination, imaging, and functional analysis.
Clinical Examination
Your dentist will begin with a thorough examination of your oral cavity, focusing on the implant site and surrounding structures.
- Visual Inspection: Looking for signs of inflammation, redness, swelling, pus, or bleeding around the implant.
- Palpation: Gently feeling the tissues around the implant to check for tenderness or swelling.
- Probing: Using a periodontal probe to measure the depth of the gum pockets around the implant. Increased pocket depths can indicate peri-implantitis.
- Mobility Check: Gently testing the implant for any movement, which could suggest failed osseointegration or a fractured implant.
- Occlusal Assessment: This is crucial for evaluating dental implant pressure pain when biting down. Your dentist will use articulating paper (a special colored paper) to check your bite. You’ll be asked to bite down, and the paper will leave marks on your teeth and the implant crown, revealing any “high spots” where excessive force is being applied. This also helps assess the overall harmony of your bite.
Imaging Techniques
Advanced imaging is indispensable for visualizing the bone structure and implant components.
- X-rays (Radiographs): Periapical and panoramic X-rays provide a two-dimensional view of the implant and surrounding bone. They can reveal:
- Bone loss around the implant, indicative of peri-implantitis.
- The position of the implant relative to vital structures like nerves and sinuses.
- Integrity of the implant components (though hairline fractures can be difficult to see).
- Cone-Beam Computed Tomography (CBCT) Scans: A CT scan and dental implants offers a detailed, three-dimensional view of the jawbone, implant, and adjacent anatomical structures. CBCT is particularly useful for:
- Accurately assessing the extent of bone loss in peri-implantitis.
- Identifying nerve impingement.
- Detecting small fractures or issues not visible on 2D X-rays.
- Evaluating sinus complications.
Differential Diagnosis
The dentist will consider all potential causes to arrive at the correct diagnosis. For example, if you report “dental implant pressure pain when biting down,” they will differentiate between:
- Mechanical issues: High bite, loose components.
- Infectious issues: Peri-implantitis, adjacent tooth abscess.
- Neurological issues: Nerve impingement.
- Sinus-related issues: Sinusitis.
This comprehensive approach ensures that the root cause of the pain is accurately identified, leading to the most appropriate and effective treatment plan.
Treatment Options for Dental Implant Pressure Pain When Biting Down
Once the cause of your dental implant pressure pain when biting down has been accurately diagnosed, your dental professional will recommend a tailored treatment plan. The approach varies significantly depending on the underlying issue.
1. Occlusal Adjustment (Bite Correction)
If the primary cause is a “high spot” or uneven bite forces, an occlusal adjustment is often the first and simplest line of treatment.
- Procedure: Your dentist will use articulating paper to identify the areas of excessive contact on your implant crown. They will then carefully and gradually reshape the surface of the crown by grinding away tiny amounts of material until your bite is balanced and comfortable. This process ensures that biting forces are evenly distributed, relieving pressure on the implant.
- Night Guard: For patients with bruxism or clenching habits, a custom-fitted night guard can be prescribed. This protective appliance cushions the biting forces, preventing damage to the implant and other teeth.
2. Treatment for Peri-Implantitis
Managing peri-implantitis requires a multi-faceted approach to control the infection and prevent further bone loss.
- Non-Surgical Debridement: For early stages, this involves thorough cleaning of the implant surface to remove plaque, calculus, and granulation tissue. Techniques may include scaling, root planing, and irrigation with antimicrobial solutions.
- Antibiotic Therapy: Local or systemic antibiotics may be prescribed to help eradicate the bacterial infection.
- Surgical Intervention: In more advanced cases with significant bone loss, surgical procedures may be necessary. These can include:
- Access Surgery: Lifting the gum tissue to gain better access to the implant surface for cleaning and decontamination.
- Decontamination: Using various methods (laser, air-abrasion, chemical agents) to thoroughly clean the infected implant surface.
- Bone Grafting: If sufficient bone loss has occurred, grafting procedures may be attempted to regenerate lost bone around the implant, improving its support and prognosis. This is a complex procedure often performed by specialists.
- Implant Removal: In severe, untreatable cases, or when the implant has become significantly mobile, removal of the implant may be the only viable option.
3. Addressing Nerve Impingement
Treatment for nerve impingement depends on its severity and the timing of diagnosis.
- Early Intervention: If nerve impingement is diagnosed soon after implant placement, sometimes removing the implant immediately can allow the nerve to recover.
- Pharmacological Management: Medications for neuropathic pain (e.g., gabapentin, tricyclic antidepressants) may be prescribed to manage symptoms.
- Surgical Decompression: In some cases, specialized surgical procedures might be considered to relieve pressure on the nerve, but these carry their own risks and are typically performed by oral and maxillofacial surgeons.
- Long-Term Management: If nerve damage is permanent, managing the chronic pain and altered sensation becomes the focus.
4. Repair or Replacement of Components
Issues with the implant’s components usually require replacement or repair.
- Loose Screw/Abutment: If a screw has loosened, it can often be simply tightened. If it’s damaged or fractured, it will need to be replaced.
- Damaged Crown: A chipped, cracked, or ill-fitting crown will need to be repaired or replaced. For details on various crown options, see abutment-supported porcelain ceramic crown.
- Fractured Implant: Unfortunately, a fractured implant post generally cannot be repaired and almost always requires removal of the entire implant.
5. Managing Sinus Issues
For implant-related sinus problems:
- Antibiotics/Decongestants: For sinus infections, antibiotics and decongestants may be prescribed.
- Surgical Correction: If the implant has perforated the sinus or if a sinus lift complication requires intervention, surgical procedures by an oral surgeon or ENT specialist may be necessary to correct the issue and, if needed, remove the implant.
6. Treating Adjacent Tooth Problems
If the pain is found to originate from an adjacent natural tooth, treatment will focus on that tooth.
- Fillings/Root Canal: For decay or infection, a filling or root canal therapy may be performed.
- Periodontal Treatment: For gum disease, deep cleaning (scaling and root planing) will be recommended.
Prevention and Long-Term Care for Dental Implants
Preventing dental implant pressure pain when biting down and ensuring the long-term success of your implants hinges on diligent home care and regular professional oversight. By adopting proactive strategies, you can significantly reduce the risk of complications.
Excellent Oral Hygiene
Maintaining impeccable oral hygiene is paramount for preventing peri-implantitis, a common cause of implant pain.
- Brushing: Brush your teeth and implants at least twice a day with a soft-bristled toothbrush. Consider an electric toothbrush, which can be more effective at removing plaque.
- Flossing: Regular flossing, or using interdental brushes specifically designed for implants, is crucial for cleaning between implants and natural teeth, and around the gum line.
- Water Flosser: A water flosser can be an excellent tool for dislodging food particles and plaque from around implants, especially in hard-to-reach areas. For recommendations, see best water flosser for dental implants.
- Antimicrobial Mouthwash: Your dentist might recommend an antimicrobial mouthwash to further reduce bacterial load. Use as directed.
- Specialized Products: Be mindful of the best toothpaste for implants and other products designed to be gentle on implant surfaces.
Regular Dental Check-ups and Professional Cleanings
Even with excellent home care, regular visits to your dentist and hygienist are indispensable.
- Frequency: Typically, professional cleanings and check-ups are recommended every six months, but your dentist might suggest more frequent visits if you have a history of periodontal disease or other risk factors.
- Professional Cleaning: Dental hygienists are trained to clean around implants using specialized tools that won’t scratch the implant surface, unlike those used for natural teeth. They will remove plaque and calculus that cannot be reached with home brushing and flossing.
- Early Detection: These visits allow your dentist to monitor the health of your implants, detect any early signs of complications like peri-implantitis or occlusal issues, and address them before they escalate into significant problems requiring more complex treatment. Early detection of dental implant bleeding or discomfort is key.
Protecting Against Bruxism and Clenching
If you grind or clench your teeth, it’s vital to protect your implants from excessive forces.
- Night Guards: As discussed, a custom-fitted night guard (occlusal guard) can absorb and distribute biting forces, significantly reducing stress on your implants and natural teeth during sleep.
- Stress Management: Exploring stress reduction techniques can also help minimize the incidence of bruxism.
Healthy Lifestyle Choices
General health also plays a role in implant longevity.
- Smoking Cessation: Smoking is a significant risk factor for peri-implantitis and can impair healing. Quitting smoking drastically improves implant prognosis.
- Balanced Diet: A healthy diet supports overall oral health. While you can eat a wide variety of foods with implants, maintaining good nutrition is beneficial. If you’re in the early stages of recovery, remember to stick to soft foods after dental implant surgery.
- Control of Systemic Conditions: Conditions like diabetes can affect healing and increase the risk of infections. Managing these conditions effectively is crucial for implant health.
Immediate Reporting of Symptoms
Never ignore any persistent discomfort, swelling, bleeding, or dental implant pressure pain when biting down.
- Don’t Wait: If you notice any changes around your implant, contact your dental office immediately. Prompt evaluation can prevent minor issues from becoming major complications, potentially saving your implant.
By adhering to these preventative measures and maintaining open communication with your dental care team, you can look forward to many years of comfortable and functional dental implants. For more information on dental implant care and services, you can always visit our main page at dentalimplantsdallastx.com/.
When to See a Dentist
While minor, temporary discomfort can sometimes occur, any persistent or increasing dental implant pressure pain when biting down should be evaluated by a dental professional without delay. Waiting can lead to the worsening of underlying issues, making treatment more complex and potentially compromising the long-term success of your implant.
You should make an appointment with your dentist if you experience any of the following:
- Persistent pain or discomfort when biting down on or around your dental implant.
- Swelling or redness of the gums surrounding the implant.
- Bleeding when brushing or flossing around the implant.
- Pus discharge from the gum tissue near the implant.
- A loose feeling in the implant, crown, or abutment.
- Numbness, tingling, or unusual sensations in your lip, chin, or tongue.
- A clicking or strange noise coming from the implant when you chew.
- Any visible change in the position of the implant or the surrounding gum tissue.
“Never ignore dental implant pressure pain when biting down. It’s your body’s way of telling you something is wrong, and early intervention is often the key to successful resolution and implant preservation.”
Remember, dental implants are a significant investment in your oral health and quality of life. Protecting that investment requires vigilance and timely professional care. If you are experiencing any concerning symptoms in 2026, contact your dental provider to schedule an evaluation.
Conclusion
Experiencing dental implant pressure pain when biting down can be a disconcerting issue, but it’s important to remember that it is often treatable, especially with early diagnosis and intervention. From occlusal overload and peri-implantitis to nerve impingement or component issues, the causes are diverse, necessitating a thorough examination by a qualified dental professional.
In 2026, advancements in dental diagnostics and treatment mean that a precise diagnosis and effective resolution are more achievable than ever. If you find yourself grappling with any discomfort or pain around your dental implant, do not hesitate. Contact your dentist immediately. Proactive communication and adherence to recommended treatment plans, coupled with meticulous oral hygiene and regular check-ups, are your best defenses against complications and your best pathway to ensuring the comfort and longevity of your dental implants. Your dental health is an ongoing journey, and our commitment is to provide you with the information and care necessary to navigate it successfully.
Actionable Next Steps:
- Schedule an Appointment: If you are experiencing dental implant pressure pain when biting down, call your dentist or oral surgeon right away.
- Be Specific: When you see your dentist, clearly describe your symptoms, including when the pain started, its intensity, and what makes it better or worse.
- Maintain Hygiene: Continue with your diligent oral hygiene routine as advised by your dentist, unless otherwise instructed.
- Avoid Hard Foods: While awaiting your appointment, try to eat softer foods and avoid chewing on the affected side to prevent further irritation.
References
- Misch, C. E. (2020). Dental Implant Prosthetics. Elsevier.
- Renvert, S., & Giovannoli, J. L. (2018). Peri-Implantitis. Quintessence Publishing Co Inc.
Dental Implant Pressure Pain Self-Assessment (2026)
This tool helps you understand potential reasons for dental implant pressure pain when biting down. It is not a substitute for professional dental advice.
1. When did you first notice the pressure pain when biting down on your dental implant?
2. Describe the nature of the pain:
3. Have you noticed any other symptoms around the implant?
4. Do you grind or clench your teeth (bruxism)?

Leave a Reply
Share your thoughts or ask a question about dental implants. Your email address will not be published.