Experiencing an unusual sensation when a dental implant feels different when chewing can be unsettling, especially after investing time and resources into restoring your smile and oral function. While dental implants are renowned for their durability and natural feel, any deviation from what’s expected or comfortable during biting or chewing warrants attention. This comprehensive guide, updated for 2026, aims to demystify why your dental implant might feel different when chewing, helping you understand potential causes, when to seek professional help, and what treatment options are available. Let’s explore the nuances of this experience and empower you with the knowledge to safeguard your oral health.
Key Takeaways
- Normal vs. Concerning Sensations: A healthy dental implant should feel like a natural tooth when chewing, albeit without the proprioceptive ‘give’ of a natural ligament. Any persistent pain, pressure, clicking, or movement is a red flag.
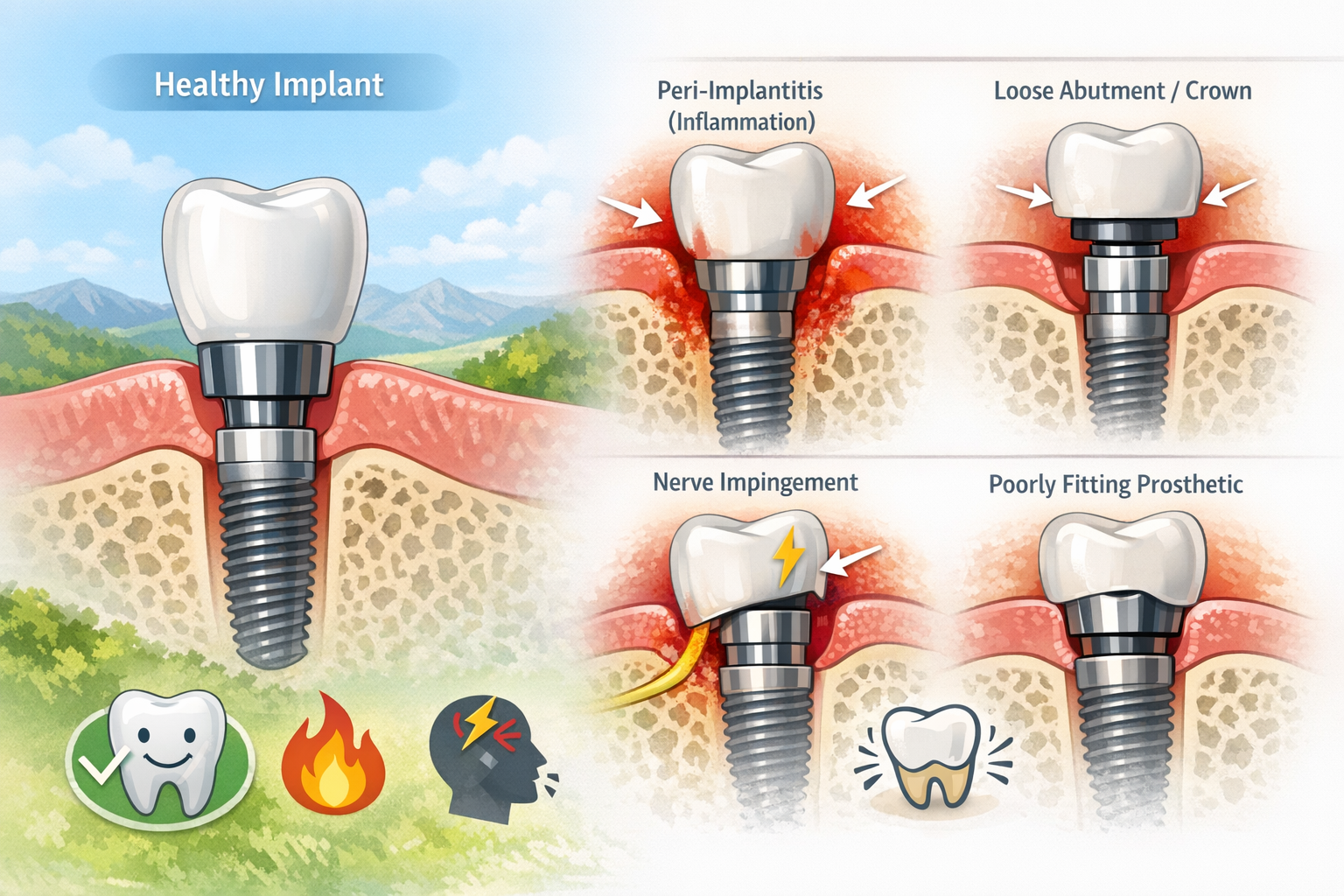
- Common Causes: Reasons for a dental implant feeling different range from minor, easily fixable issues like a loose screw or occlusal imbalance, to more serious concerns like peri-implantitis, nerve damage, or implant failure.
- Importance of Prompt Action: Ignoring changes in sensation can lead to more significant complications, potentially jeopardizing the implant’s longevity and your overall oral health. Early diagnosis and intervention are crucial.
- Diagnostic Tools: Dentists use a variety of tools, including clinical examination, X-rays, and 3D imaging, to accurately pinpoint the cause of discomfort.
- Treatment Varies: Solutions depend entirely on the underlying problem, from simple adjustments to more complex procedures like infection treatment or implant replacement.
Why Your Dental Implant Feels Different When Chewing: Unpacking the Causes
It’s natural to have questions if your dental implant feels different when chewing. The goal of a dental implant is to mimic a natural tooth, providing stable and comfortable chewing function. However, unlike natural teeth, implants fuse directly with the bone and lack the periodontal ligament that provides natural teeth with a subtle sense of touch, pressure, and movement. This difference means that while a successful implant should feel strong and secure, it won’t have the exact same sensory feedback as a natural tooth. Therefore, any new or concerning difference in sensation when chewing with your implant should be investigated.
Understanding the Normal vs. Abnormal Sensation
Before diving into potential problems, let’s clarify what’s generally considered normal. A properly integrated and restored dental implant should allow you to chew foods with confidence and comfort. You should not experience:
- Sharp pain
- Constant pressure
- Clicking or popping sounds
- Wobbling or movement
- Sensitivity to hot or cold (unless other natural teeth are involved)
- A feeling of something “off” or “unstable”
If your dental implant feels different when chewing in any of these ways, it’s time to consult your dental professional.
Common Reasons for a Dental Implant Feeling Different When Chewing
Several factors, ranging from minor to severe, can contribute to a changed sensation in your dental implant. Let’s explore these in detail.
1. Occlusal Imbalance (Bite Issues)
One of the most frequent reasons a dental implant feels different when chewing is an improper bite or occlusal imbalance. If the implant crown is slightly too high or makes contact with opposing teeth prematurely or excessively during chewing, it can create undue pressure.
- How it feels: This often manifests as a feeling of the implant hitting first, a persistent pressure, or even soreness in the surrounding teeth or jaw joint. It can make chewing feel awkward or uncomfortable.
- Why it happens: Minor shifts in your bite can occur over time, or the initial crown placement might have been slightly off. Even a small discrepancy can cause significant issues due to the rigid nature of the implant-bone connection.
- Solution: Your dentist can easily adjust the biting surface of the implant crown to ensure it integrates seamlessly with your natural bite. This is a common and usually quick fix.
2. Loose Abutment or Crown
The dental implant system comprises three main parts: the implant screw (fixtures), the abutment (connector), and the crown (the visible tooth). If the abutment or the crown becomes loose, it can definitely make your dental implant feels different when chewing.
- How it feels: You might notice a subtle movement, a clicking sound, or a sensation that the tooth is “wobbly.” Food might get caught more easily around the crown. You might also experience mild discomfort or a feeling of instability.
- Why it happens: The small screws that secure the abutment to the implant, or the crown to the abutment, can sometimes loosen over time due to normal chewing forces. Less commonly, the cement bonding the crown to the abutment might fail.
- Solution: Your dentist can typically tighten the screw or re-cement the crown. This is usually a straightforward procedure. Sometimes, a new screw might be needed if the old one is damaged. Understanding the role of the abutment placement and the abutment-supported porcelain ceramic crown can help in comprehending this issue.
3. Peri-implantitis: Infection Around the Implant
Peri-implantitis is an inflammatory condition affecting the tissues surrounding a dental implant, leading to bone loss. It’s akin to periodontal disease in natural teeth and is a more serious cause for concern.
- How it feels: You might experience throbbing pain, tenderness, swelling, redness of the gums around the implant, or a bad taste in your mouth. When chewing, the pressure can exacerbate these symptoms, making the implant feel unstable or painful.
- Why it happens: Poor oral hygiene is the primary culprit, allowing bacteria to accumulate around the implant, leading to inflammation and infection. Smoking, uncontrolled diabetes, and a history of periodontitis also increase risk.
- Solution: Treatment depends on the severity. Early stages might involve deep cleaning and antibiotics. More advanced cases may require surgical intervention to decontaminate the implant surface and potentially regenerate bone. Prevention through meticulous oral hygiene is paramount. Learn more about comprehensive dental implant aftercare instructions to prevent such issues.
4. Nerve Impingement or Damage
While rare, nerve damage during the implant placement surgery can manifest as altered sensation, including when your dental implant feels different when chewing.
- How it feels: This can range from numbness, tingling, burning, or a heightened, painful sensitivity in the area of the implant, which can become more noticeable during chewing. It might feel like a persistent ache or an electric shock.
- Why it happens: If the implant is placed too close to a nerve canal, or if the drilling process causes trauma to the nerve, it can result in nerve impingement or damage. This is more common with implants in the lower jaw near the inferior alveolar nerve.
- Solution: If diagnosed early, removal of the implant or revision surgery might be considered. In some cases, the nerve may heal on its own, but persistent symptoms require specialist evaluation.
5. Implant Fracture or Failure
Although dental implants are incredibly strong, in very rare instances, the implant itself can fracture, or the bone around it might fail to integrate or even resorb, leading to implant failure.
- How it feels: A fractured implant would typically cause significant pain, instability, and an inability to chew on that side. Implant failure due to lack of osseointegration or significant bone loss would present as a loose or mobile implant, often accompanied by pain and swelling.
- Why it happens: Excessive forces on the implant (e.g., severe bruxism or clenching), trauma, poor bone quality, or certain medical conditions can contribute to implant fracture or failure.
- Solution: Unfortunately, a fractured implant usually necessitates its removal. For implant failure, the implant will need to be removed, and the site allowed to heal. Often, a bone graft may be required before a new implant can be placed. This process highlights the importance of understanding the full dental implant recovery timeline.
6. Adjacent Tooth Issues
Sometimes, the problem isn’t with the implant itself but with an adjacent natural tooth.
- How it feels: You might perceive the discomfort as coming from the implant area when it’s actually an adjacent tooth experiencing decay, a crack, or gum disease. The sensation when chewing could be sharp or sensitive.
- Why it happens: Dental problems in neighboring teeth are independent of the implant but can be easily mistaken for implant-related issues.
- Solution: A thorough dental examination will identify if the problem lies with a natural tooth, which can then be treated accordingly.
7. Sinus Issues (for upper jaw implants)
For implants placed in the upper jaw, particularly in the molar and premolar regions, proximity to the maxillary sinuses can sometimes lead to issues.
- How it feels: You might experience pressure, discomfort, or a feeling of fullness in the sinus area when chewing, especially if the implant has penetrated the sinus cavity or caused inflammation.
- Why it happens: Inadequate bone height in the upper jaw often necessitates a sinus lift procedure. If the implant extends into the sinus or an infection develops, it can cause problems.
- Solution: Treatment could involve antibiotics for infection, or in more severe cases, surgical intervention to address the implant’s position relative to the sinus.
When to See Your Dentist About Your Dental Implant Feeling Different When Chewing
It’s crucial to understand that any persistent or concerning change in how your dental implant feels when chewing should prompt a visit to your dentist or oral surgeon. Do not wait for the symptoms to worsen. Early intervention can often prevent more serious complications and ensure the longevity of your implant.
Symptoms That Demand Immediate Attention
- Severe or increasing pain: Especially if it doesn’t subside with over-the-counter pain relievers.
- Visible movement or wobbling: Any noticeable motion of the crown, abutment, or the implant itself.
- Swelling, redness, or pus: Signs of infection around the implant site.
- Fever or general malaise: Systemic signs of infection.
- Numbness or persistent tingling: This could indicate nerve involvement.
- Difficulty chewing or speaking: If the sensation significantly impacts your daily functions.
Your dental professional is the best person to diagnose the exact cause of your discomfort. They have the expertise and diagnostic tools to thoroughly assess the situation.
The Diagnostic Process
When you visit your dentist regarding a dental implant that feels different when chewing, here’s what you can typically expect:
- Clinical Examination: The dentist will visually inspect the implant, surrounding gums, and adjacent teeth. They will check for signs of inflammation, bleeding, or pus. They’ll also assess the stability of the crown and abutment.
- Bite Assessment: They will evaluate your bite to see if the implant crown is experiencing premature or excessive contact, which could be causing occlusal trauma.
- Radiographic Imaging:
- X-rays: Standard dental X-rays (periapical, panoramic) are essential to visualize the implant, the surrounding bone, and check for bone loss, fractures, or problems with integration.
- 3D Cone Beam CT (CBCT): For a more detailed assessment, especially if nerve impingement or sinus involvement is suspected, a 3D CBCT scan provides a comprehensive view of the bone structure, implant position, and nerve pathways.
- Probing and Periodontal Charting: Similar to natural teeth, the gum tissue around the implant will be gently probed to check for pocket depths, which can indicate peri-implantitis.
- Patient History: Your dentist will ask about your symptoms, when they started, what makes them better or worse, and your overall health history, including any medications you’re taking.
This thorough diagnostic approach allows your dental team to accurately pinpoint why your dental implant feels different when chewing and formulate an effective treatment plan. For more information on dental implant consultation, visit our dental implant consultation page.
Treatment Options for a Dental Implant that Feels Different When Chewing
The treatment approach will be entirely dependent on the underlying cause identified during the diagnostic process. Here’s a look at potential interventions:
1. Occlusal Adjustment
- Problem: High spot on the crown causing premature contact.
- Treatment: The dentist will carefully polish and reshape the biting surface of the implant crown to relieve pressure and restore a balanced bite. This is a non-invasive and usually quick procedure.
2. Tightening or Replacement of Components
- Problem: Loose abutment screw or crown.
- Treatment: The dentist will access the screw (often by removing the crown or an access cover) and gently tighten it to the recommended torque specifications. If the crown was cemented, it might be re-cemented. In cases of a stripped or damaged screw, it will be replaced.
3. Management of Peri-implantitis
- Problem: Infection and inflammation around the implant.
- Treatment:
- Non-Surgical: Early stages may involve thorough debridement (cleaning) of the implant surface, irrigation with antimicrobial solutions, and prescription antibiotics.
- Surgical: More advanced cases often require surgical intervention. This can include flap surgery to gain access to the implant surface for thorough cleaning, bone grafting (if significant bone loss has occurred, as discussed in bone grafts for dental implants), and soft tissue grafting to improve gum health around the implant. Regular follow-up and meticulous home care are crucial post-treatment.
4. Addressing Nerve Issues
- Problem: Nerve impingement or damage.
- Treatment: This is a complex issue. Depending on the severity and duration of symptoms, options may include:
- Monitoring: For mild, transient symptoms, the nerve may heal on its own.
- Medication: Nerve pain medications may be prescribed to manage symptoms.
- Surgical Intervention: In severe cases, particularly if the implant is directly impinging on the nerve, surgical removal of the implant may be necessary. Nerve repair surgery might be considered, though success rates vary.
5. Implant Removal and Replacement
- Problem: Implant fracture, irreversible peri-implantitis, or complete failure of osseointegration.
- Treatment: The failed implant will need to be surgically removed. The area will then be allowed to heal. Often, a bone graft recovery dental implant procedure is necessary to rebuild sufficient bone volume before a new implant can be considered. After adequate healing, a new implant can be placed. This process emphasizes the long-term commitment and detailed planning involved in successful dental implantology, as offered by practices like Dental Implants Dallas TX.
6. Treating Adjacent Tooth Pathology
- Problem: Decay, crack, or gum disease in a neighboring natural tooth.
- Treatment: The adjacent tooth will be treated for its specific problem, which might involve a filling, root canal therapy, or periodontal treatment. Once the natural tooth is healthy, the perceived discomfort around the implant should resolve.
7. Sinus Management
- Problem: Implant-related sinus issues.
- Treatment: If an infection is present, antibiotics will be prescribed. If the implant is too far into the sinus cavity and causing chronic problems, it might need to be repositioned or removed, and the sinus membrane repaired.
Preventing Future Issues with Your Dental Implant

While some complications are unpredictable, many reasons why a dental implant feels different when chewing can be prevented through diligent care and regular dental visits.
- Maintain Excellent Oral Hygiene: This is paramount. Brush at least twice a day with a soft-bristled brush, floss daily (or use an interdental brush specifically designed for implants), and use an antimicrobial mouthwash if recommended. Focus on cleaning around the gum line of the implant.
- Regular Dental Check-ups: Visit your dentist for professional cleanings and examinations typically every six months, or as advised. These appointments allow your dental team to monitor your implant’s health, check your bite, and detect any potential issues early.
- Avoid Hard and Sticky Foods (Initially): Especially during the initial healing phases, adhere strictly to your dentist’s dietary recommendations. Even after full integration, avoid excessively hard foods that could damage the crown or place undue stress on the implant. A guide like 50 soft foods after dental implant can be very helpful.
- Address Bruxism (Teeth Grinding): If you grind or clench your teeth, inform your dentist. They may recommend a nightguard to protect your implants and natural teeth from excessive forces.
- Quit Smoking: Smoking significantly increases the risk of peri-implantitis and implant failure.
- Manage Systemic Health Conditions: Conditions like diabetes can affect healing and increase the risk of infection. Keep any chronic health conditions well-managed.
- Choose an Experienced Dental Professional: The skill and experience of your oral surgeon and restorative dentist play a crucial role in the long-term success of your implants. Ensure you’re working with a team well-versed in implant dentistry, such as the experts mentioned on our about us page.
By taking these proactive steps, you can significantly reduce the likelihood of experiencing discomfort and ensure your dental implant remains a functional and comfortable part of your smile for many years to come.
Conclusion
Experiencing a sensation where your dental implant feels different when chewing can be concerning, but it’s important to remember that most issues are treatable, especially when caught early. From minor bite adjustments to addressing peri-implantitis or component loosening, a range of solutions exists. The key is not to ignore persistent discomfort or unusual sensations.
If you notice your dental implant feels different when chewing, whether it’s pain, pressure, clicking, or instability, contact your dental professional without delay. A thorough examination, including advanced imaging, will help pinpoint the exact cause. With prompt and appropriate intervention, you can restore comfort and confidence in your dental implant, ensuring it continues to provide the functional and aesthetic benefits you expect. Prioritize your oral health in 2026 by being vigilant and proactive about any changes in your dental implants.
References
[1] Mombelli, A. (2018). Peri‐implantitis. Current Oral Health Reports, 5(2), 106-114.
[2] Misch, C. E. (2008). Contemporary implant dentistry. Mosby Elsevier.
Use this tool to help understand potential reasons if your dental implant feels different when chewing. This is for informational purposes only and does not replace professional dental advice.
Disclaimer: This tool provides general information and is not a substitute for professional dental diagnosis or treatment. Always consult with a qualified dental professional for any concerns about your dental implants.

Leave a Reply
Share your thoughts or ask a question about dental implants. Your email address will not be published.