Undergoing dental implant surgery is a significant step towards restoring your smile and oral health. While highly successful, it’s natural to anticipate some level of discomfort during the recovery phase. Understanding how to manage and achieve effective pain relief after dental implants is crucial for a smooth and comfortable healing process. This comprehensive guide, crafted by an expert SEO content strategist and senior editor, will walk you through everything you need to know, from expected discomfort to advanced pain management strategies, ensuring you’re well-prepared for your recovery in 2026 and beyond.
Key Takeaways
- Expected Discomfort is Normal: Mild to moderate pain, swelling, and bruising are common after dental implant surgery and are typically manageable with medication.
- Follow Post-Operative Instructions Diligently: Adhering to your dentist’s or oral surgeon’s instructions is paramount for effective pain relief and optimal healing.
- Utilize a Combination of Strategies: A mix of pharmacological (medication) and non-pharmacological (cold compresses, rest) methods often provides the best results for managing discomfort.
- Know When to Contact Your Dentist: Persistent, severe, or worsening pain, fever, or excessive bleeding are signs that require immediate professional attention.
- Healing is a Gradual Process: Complete healing takes time, and consistent care, including a soft diet and good oral hygiene, contributes significantly to long-term comfort and success.
Understanding Post-Operative Discomfort: What to Expect

The decision to get dental implants is an investment in your long-term oral health, offering a permanent solution for missing teeth. As with any surgical procedure, some level of post-operative discomfort is to be expected. It’s important to differentiate between normal post-surgical sensations and signs that might indicate a complication. Knowing what to expect regarding pain relief after dental implants can help you prepare mentally and physically for the recovery period.
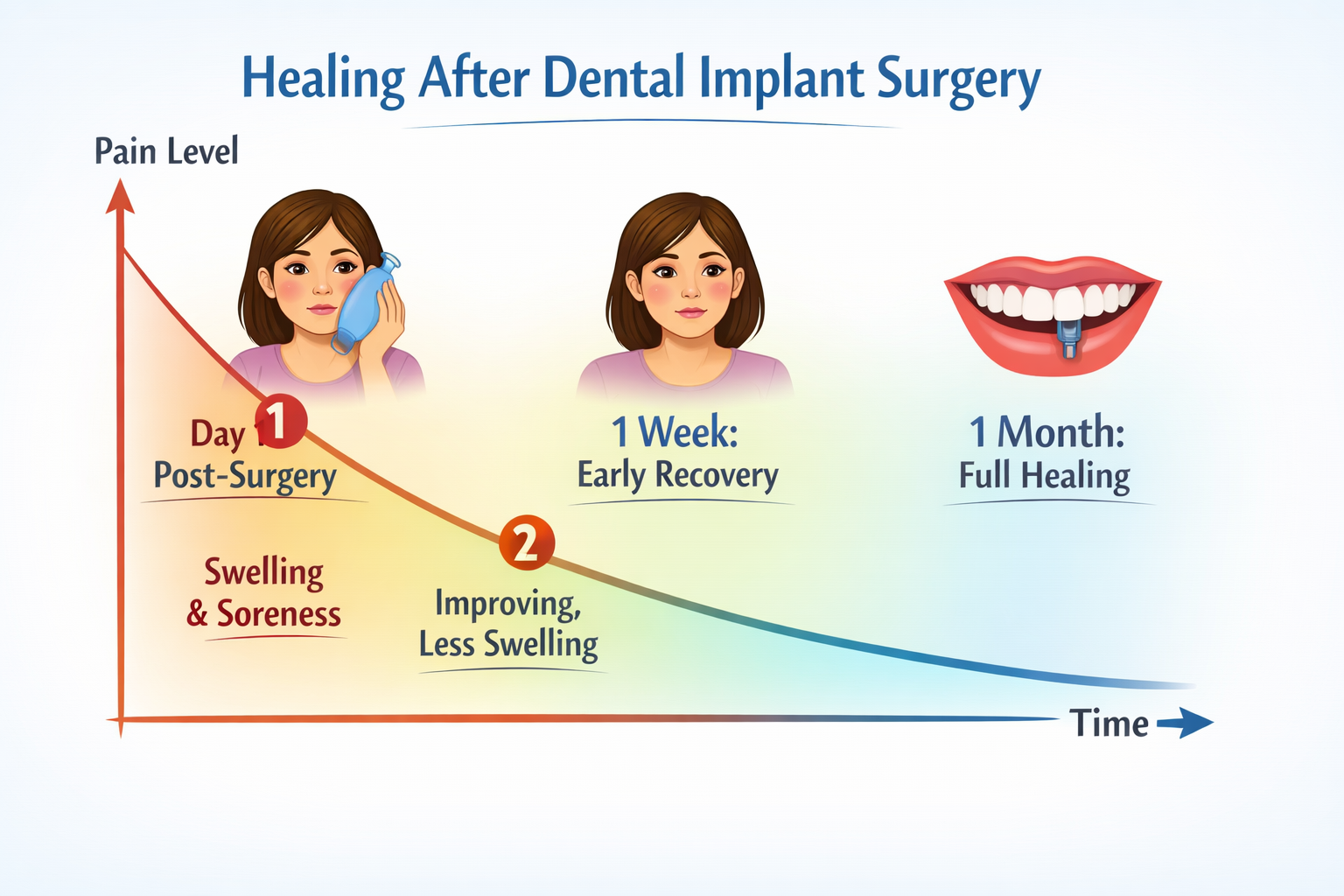
Immediately after the surgery, once the local anesthetic wears off, you will likely begin to feel some soreness. This discomfort typically peaks within the first 24 to 72 hours and gradually subsides over the next few days to a week. The intensity of pain can vary significantly from person to person, influenced by factors such as the number of implants placed, the complexity of the procedure (e.g., whether bone grafting was also performed), and individual pain tolerance.
Common Post-Operative Symptoms
Here’s a breakdown of the typical symptoms you might experience:
- Pain or Soreness: This is the most common symptom. It can range from a dull ache to moderate pain. Your dental professional will likely prescribe or recommend pain medication to manage this.
- Swelling: Swelling around the surgical site, face, and jaw is very common. It usually peaks 2-3 days after surgery and then slowly decreases.
- Bruising: You might notice some bruising on your face and neck. This is normal and will resolve on its own.
- Minor Bleeding: Slight oozing or intermittent bleeding from the surgical site is normal for the first 24-48 hours.
- Discomfort When Opening Mouth: Stiffness or soreness in the jaw muscles can make it difficult to open your mouth wide.
- Numbness: Residual numbness from the local anesthetic might linger for a few hours. In rare cases, nerve irritation can cause prolonged numbness, which should be reported to your dentist.
“While the thought of dental implant surgery might seem daunting, modern techniques and effective pain management strategies ensure that the procedure itself is often less uncomfortable than anticipated, and post-operative pain is typically manageable.”
It’s crucial to remember that while these symptoms are normal, they should gradually improve over time. If your pain worsens significantly after a few days, or if you develop new, concerning symptoms, it’s essential to contact your dental professional immediately. For more information on what to expect during recovery, you can explore our guide on complete dental implant recovery timeline.
Pharmacological Approaches to Pain Relief After Dental Implants
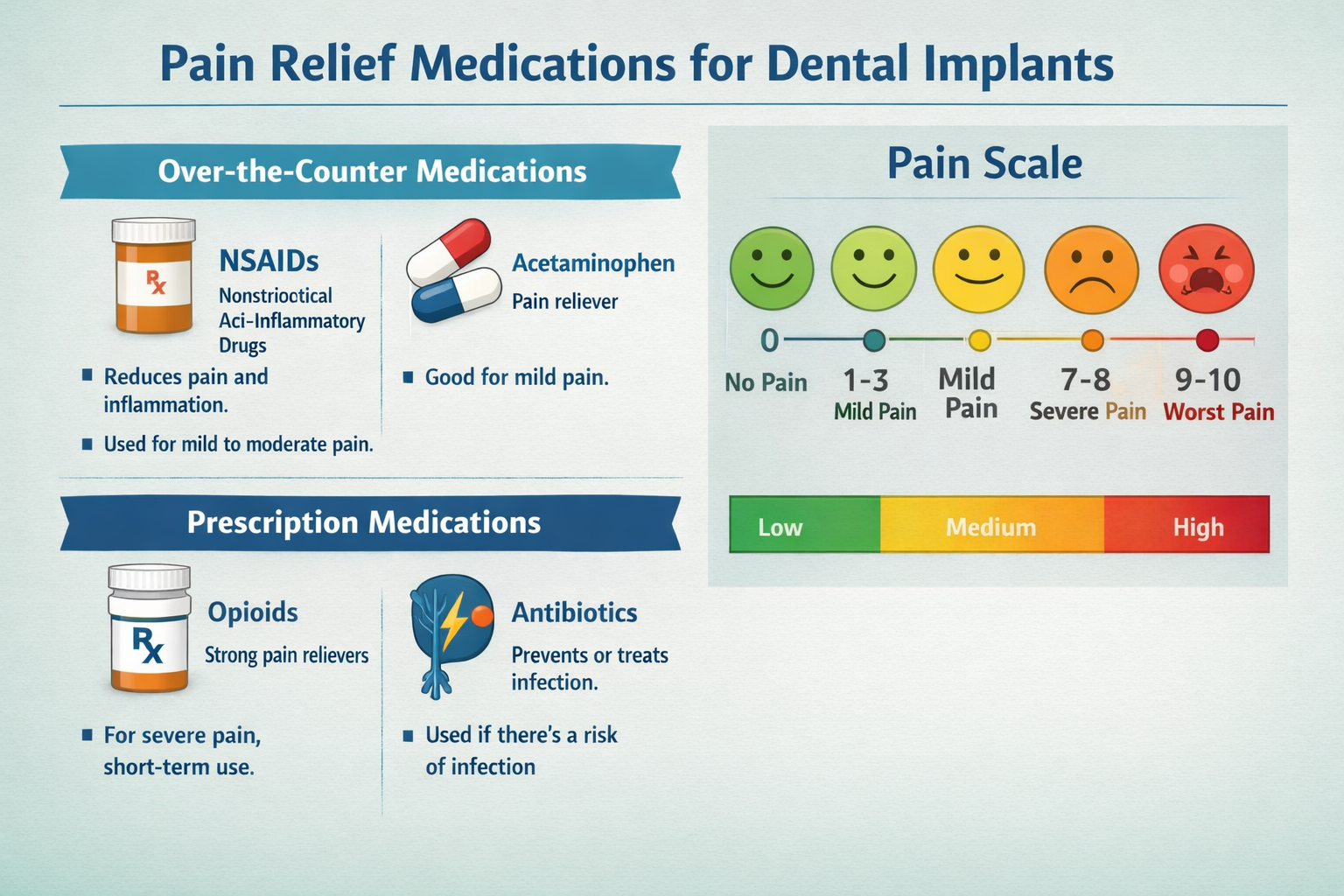
Effective pain relief after dental implants often involves a combination of over-the-counter and prescription medications. Your dental surgeon will provide specific recommendations tailored to your individual needs and the extent of your procedure. It’s vital to follow these instructions precisely to manage discomfort, reduce inflammation, and prevent complications.
Over-the-Counter (OTC) Pain Relievers
For mild to moderate pain, OTC medications are often sufficient. These generally fall into two categories:
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs):
- Ibuprofen (Advil, Motrin): Often the first line of defense due to its pain-relieving and anti-inflammatory properties. It can significantly reduce swelling and pain.
- Naproxen (Aleve): Similar to ibuprofen, naproxen offers longer-lasting pain relief, typically taken every 8-12 hours.
- Dosage and Frequency: Always follow the package instructions or your dentist’s specific advice. Taking NSAIDs with food can help prevent stomach upset.
Acetaminophen (Tylenol):
- This medication primarily reduces pain and fever but does not have significant anti-inflammatory effects. It can be a good option if you cannot take NSAIDs or in combination with NSAIDs for enhanced pain control.
- Dosage and Frequency: Adhere strictly to recommended doses to avoid liver damage.
Your dentist might suggest alternating between ibuprofen and acetaminophen every few hours. For example, taking ibuprofen, then three hours later taking acetaminophen, and so on. This approach can provide more consistent pain relief by targeting different pain pathways and keeping overall discomfort at bay.
Prescription Pain Medications
For more severe pain, your oral surgeon may prescribe stronger medications. These are typically used for the first few days post-surgery when discomfort is at its peak.
- Opioid Pain Relievers (e.g., Hydrocodone, Oxycodone):
- These are potent pain medications prescribed for short-term use. They work by changing how your brain and nervous system respond to pain.
- Important Considerations: Opioids can cause side effects like drowsiness, nausea, constipation, and dizziness. They also carry a risk of dependence, so use them strictly as prescribed and only for the shortest duration necessary. Do not drive or operate heavy machinery while taking opioids.
- Prescription Strength NSAIDs:
- Sometimes, a higher-dose prescription NSAID might be given for its enhanced anti-inflammatory and pain-relieving effects.
Antibiotics and Anti-Inflammatories
Beyond pain relief, your dental professional might also prescribe other medications to aid in your recovery and prevent complications:
- Antibiotics: Often prescribed to prevent infection, which is crucial for the success of your dental implant. It’s imperative to take the entire course of antibiotics as directed, even if you start feeling better. Find out more about antibiotics after dental implant surgery.
- Corticosteroids (e.g., Dexamethasone): In some cases, a short course of corticosteroids might be prescribed to significantly reduce swelling and inflammation, thereby contributing to overall pain relief.
Table 1: Common Medications for Pain Relief After Dental Implants
| Medication Type | Examples | Primary Action | Considerations |
|---|---|---|---|
| OTC NSAIDs | Ibuprofen, Naproxen | Pain relief, anti-inflammatory | Take with food; check for contraindications (e.g., blood thinners) |
| OTC Analgesics | Acetaminophen | Pain relief, fever reducer | No anti-inflammatory; avoid exceeding daily limits |
| Prescription Opioids | Hydrocodone, Oxycodone | Strong pain relief | Sedation, nausea, constipation; risk of dependence; short-term use only |
| Antibiotics | Amoxicillin, Clindamycin | Prevent infection | Complete the full course; watch for allergic reactions |
| Corticosteroids | Dexamethasone | Reduce swelling, inflammation | Short-term use; specific dosing instructions |
Always discuss any existing medical conditions, allergies, or other medications you are taking with your dental professional before surgery. This ensures that the prescribed regimen for pain relief after dental implants is safe and effective for you.
Non-Pharmacological Strategies for Pain Relief and Healing

While medications are vital for managing pain, several non-pharmacological strategies can significantly contribute to pain relief after dental implants and promote faster, more comfortable healing. These methods often complement medication, reducing reliance on stronger drugs and enhancing overall well-being during recovery.
Cold and Heat Therapy
- Cold Compresses (First 24-48 Hours): Applying ice packs or cold compresses to the outside of your face, over the surgical site, is highly effective in reducing swelling and bruising.
- Method: Apply for 15-20 minutes, then remove for 15-20 minutes. Repeat this cycle for the first day or two. This constricts blood vessels, minimizing inflammation.
- Moist Heat (After 48 Hours): If swelling persists after the initial 48 hours, some dental professionals may recommend applying moist heat.
- Method: Use a warm, moist towel for 20 minutes on, 20 minutes off. This can help improve blood circulation and reduce stiffness, but only if swelling has stabilized or begun to decrease. Always consult your dentist before applying heat.
Rest and Elevation
- Adequate Rest: Your body needs energy to heal. Prioritize rest, especially during the first few days after surgery. Avoid strenuous activities that could increase blood pressure or dislodge the blood clot, which is crucial for healing.
- Elevate Your Head: When resting or sleeping, keep your head elevated with extra pillows. This helps to minimize swelling and reduce throbbing at the surgical site.
Diet and Hydration
- Soft Food Diet: Sticking to a soft food diet is paramount to prevent irritation or damage to the surgical site. Foods like yogurt, smoothies, mashed potatoes, and soups are excellent choices. Avoid crunchy, hard, chewy, or spicy foods for several weeks. Learn more about soft foods after dental implant surgery.
- Hydration: Drink plenty of fluids, especially water. Avoid alcohol and caffeinated beverages, as they can interfere with healing and hydration.
- Avoid Straws: The sucking action required to use a straw can create negative pressure in your mouth, potentially dislodging the blood clot and leading to a painful condition called “dry socket.”
Oral Hygiene
Maintaining excellent oral hygiene is crucial, but gently.
- Gentle Rinsing: Your dentist will likely recommend using a prescribed antimicrobial mouthwash (like chlorhexidine) or a warm salt water rinse starting 24 hours after surgery.
- Method: Gently swish the rinse, do not vigorously spit, as this can dislodge the blood clot. Let it gently trickle out of your mouth.
- Careful Brushing: Brush your teeth gently, avoiding the surgical site directly for the first few days. You can carefully clean the teeth away from the surgical area.
- Avoid Irritants: Refrain from smoking or using tobacco products. Smoking significantly hinders healing and increases the risk of complications, including infection and implant failure [1]. You should also avoid alcohol for at least a week after surgery, as it can delay healing and interact with medications. Read more about alcohol after dental implant surgery.
Stress Reduction
Anxiety and stress can heighten pain perception. Incorporating stress-reducing activities can be beneficial:
- Mindfulness and Deep Breathing: Gentle breathing exercises can help you relax and manage discomfort.
- Distraction: Engage in light activities like reading, watching movies, or listening to music to take your mind off the pain.
By integrating these non-pharmacological methods with your prescribed medications, you can achieve comprehensive pain relief after dental implants and support a quicker, more comfortable recovery.
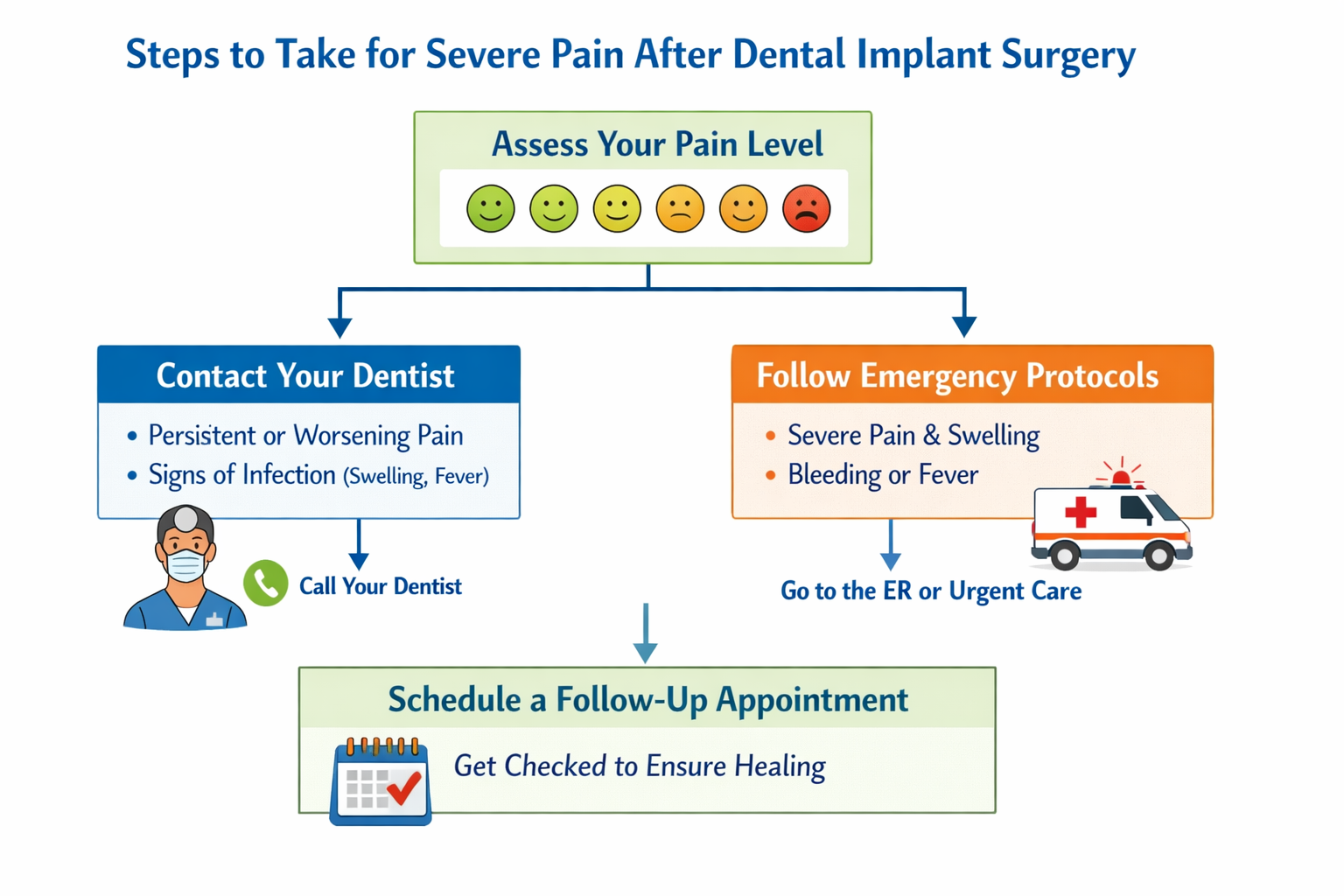
When to Contact Your Dentist: Recognizing Warning Signs
While some discomfort is a normal part of the healing process after dental implant surgery, it’s crucial to know when your symptoms indicate a potential complication that requires immediate professional attention. Being proactive can prevent minor issues from becoming major problems and ensure the long-term success of your implant.
Signs of Normal Recovery vs. Complications
It can be challenging to distinguish between expected post-operative symptoms and warning signs. Here’s a general guideline:
| Symptom | Normal Recovery | Warning Sign (Contact Your Dentist) |
|---|---|---|
| Pain | Mild to moderate, gradually decreasing over days. | Severe pain that worsens significantly after 3-5 days; throbbing, unbearable pain; pain unresponsive to medication. |
| Swelling | Peaks at 2-3 days, gradually decreases. | Increasing swelling after 3 days; swelling that spreads rapidly to other facial areas. |
| Bleeding | Slight oozing, intermittent, for 24-48 hours. | Heavy, continuous bleeding that doesn’t stop with pressure. |
| Fever | Low-grade fever (up to 100°F/37.8°C) in first 24h. | High fever (above 101°F/38.3°C) or fever accompanied by chills. |
| Numbness | Temporary, residual from local anesthetic. | Persistent numbness, tingling, or altered sensation that lasts for more than 24 hours after anesthetic should have worn off. |
| Discharge/Taste | Minor metallic taste due to blood. | Pus-like discharge from the surgical site; foul taste or odor. |
Specific Situations Requiring Immediate Attention
- Uncontrolled Bleeding: If you experience heavy bleeding that doesn’t subside after applying firm pressure with gauze for 30 minutes, contact your dentist or oral surgeon immediately.
- Increasing or Severe Pain: If your pain intensifies significantly after the first few days, or if it’s severe and not relieved by prescribed medications, this could indicate an infection or other complication.
- Spreading Swelling: While some swelling is normal, if it spreads rapidly to your neck, throat, or eye, or if it becomes hard and tender, seek immediate help.
- High Fever or Chills: These are classic signs of infection.
- Prolonged Numbness: Numbness that persists for more than 24 hours after the local anesthetic should have worn off could indicate nerve involvement and needs to be evaluated.
- Allergic Reaction: If you develop a rash, hives, difficulty breathing, or severe itching after taking medication, seek emergency medical care immediately.
- Implant Mobility: While rare, if you notice the implant feels loose or moves, contact your dentist immediately.
“Managing minor bleeding after dental implants is part of normal post-operative care, but persistent or excessive bleeding is a red flag that warrants immediate professional evaluation.”
It’s always better to err on the side of caution. If you are concerned about any symptom, even if it seems minor, do not hesitate to contact your dental professional. They are your best resource for guidance and can assess whether your symptoms are normal or require intervention. Your dental team is dedicated to ensuring your comfort and successful recovery, especially concerning pain relief after dental implants. If you have questions about your specific treatment, you can always reach out to your provider, or learn more about us at Dental Implants Dallas TX.
Long-Term Comfort and Maintaining Your Dental Implants
Achieving immediate pain relief after dental implants is just the beginning. Long-term comfort and the success of your implants depend heavily on meticulous aftercare and regular maintenance. Even after the initial healing period, ongoing care ensures your implants integrate well, last a lifetime, and remain free from complications.
The Osseointegration Process
Dental implants work because they fuse directly with your jawbone in a process called osseointegration. This process is crucial for the implant’s stability and strength, allowing it to function like a natural tooth root. While the initial surgical site heals within a few weeks, osseointegration can take several months (typically 3-6 months, sometimes longer) [2]. During this time, it’s vital to:
- Avoid putting excessive pressure on the implant: Follow your dentist’s instructions regarding chewing limitations. For instance, if you’ve had a provisional crown placed, avoid biting down on very hard foods.
- Maintain excellent oral hygiene: Keep the area around the implant clean to prevent infection that could jeopardize osseointegration.
Transitioning to Permanent Restorations
Once osseointegration is complete, the abutment (a connector piece) is placed, followed by the permanent crown, bridge, or denture. You may experience minor discomfort or sensitivity after the abutment placement, but this is typically much less severe than the initial surgery and resolves quickly. This is a significant milestone in your journey towards complete oral restoration and full long-term comfort.
Ongoing Oral Hygiene for Implant Longevity
Maintaining your dental implants is similar to caring for your natural teeth, but with a few important distinctions:
- Regular Brushing: Brush twice daily with a soft-bristled toothbrush. You may need to use an implant-specific brush or technique.
- Flossing: Floss daily, paying special attention to the areas around your implants. Non-abrasive dental tape or an interdental brush can be effective. Consider using a water flosser specifically designed for dental implants for thorough cleaning around the implant posts.
- Specialized Mouthwash: Your dentist might recommend a non-alcoholic, antimicrobial mouthwash to help control bacteria.
- Professional Cleanings: Regular check-ups and professional cleanings (typically every 6 months) are essential. Dental hygienists use specialized tools designed for implants to prevent damage and remove plaque and tartar buildup that can lead to peri-implantitis (a gum disease similar to periodontitis that affects implants).
Addressing Potential Long-Term Discomfort
While dental implants are highly successful, rare long-term issues can arise that might cause discomfort:
- Peri-implantitis: Inflammation and infection around the implant, which can lead to bone loss. Symptoms include redness, swelling, bleeding, and tenderness around the implant. Early detection and treatment are crucial.
- Loose Abutment or Crown: If the crown or abutment loosens, it can cause discomfort or affect your bite. This usually requires a simple adjustment by your dentist.
- Nerve Damage: Although rare, persistent numbness, tingling, or pain in the lip, tongue, or chin area could indicate nerve irritation or damage. This usually manifests soon after surgery, but it’s important to report any new or persistent symptoms.
- Implant Failure: In rare cases, the implant may not integrate with the bone or can fail later due to infection, trauma, or poor bone quality. This would necessitate removal of the implant and consideration of further treatment.
Regular communication with your dental professional is key to addressing any concerns promptly. By adhering to a diligent oral hygiene routine and attending regular check-ups, you significantly increase the chances of long-term success and continuous comfort with your dental implants. This proactive approach is the best strategy for lasting pain relief after dental implants and a healthy, beautiful smile for years to come.
Dental Implant Pain Management Guide
This interactive tool helps you understand potential pain levels and recommended strategies after dental implant surgery. Remember, this is for informational purposes only and not a substitute for professional medical advice.
Your Post-Op Status
Recommendations
Adjust the settings above to see tailored pain management advice.
Disclaimer: This tool provides general guidance. Always follow the specific instructions from your dental surgeon regarding pain relief after dental implants and contact them if you have any concerns about your recovery.
Conclusion
Navigating the recovery period after dental implant surgery is a critical phase in ensuring the success and longevity of your new smile. While some discomfort is a natural part of the healing process, effective pain relief after dental implants is entirely achievable through a combination of diligent post-operative care, appropriate medication, and sensible lifestyle choices. Remember that your journey to a fully restored smile is a process, and patience, along with adherence to professional advice, will lead to the best outcomes.
From managing initial swelling with cold compresses to carefully choosing a soft diet, every step you take contributes to a smoother, more comfortable recovery. It is imperative to distinguish between normal healing sensations and potential warning signs. When in doubt, always err on the side of caution and reach out to your dental professional. They are your most valuable resource and are equipped to provide personalized guidance and intervention when necessary.
By following the comprehensive advice provided in this guide, and maintaining open communication with your dental team, you can confidently approach your recovery in 2026. Your commitment to proper aftercare will not only ensure effective pain relief but also the long-term health and stability of your dental implants, allowing you to enjoy the benefits of a complete and healthy smile for many years to come.
Actionable Next Steps:
- Review Post-Operative Instructions: Re-read and ensure you fully understand all instructions provided by your dental surgeon. Keep their emergency contact information handy.
- Prepare Your Recovery Space: Stock up on recommended soft foods, pain relievers, and cold compresses before your surgery.
- Adhere to Medication Schedules: Take all prescribed medications (painkillers, antibiotics) exactly as directed, even if you start feeling better.
- Practice Gentle Oral Hygiene: Follow specific instructions for brushing and rinsing to keep the surgical site clean without disturbing it.
- Monitor Your Symptoms: Pay close attention to your pain levels, swelling, and any unusual symptoms.
- Attend Follow-Up Appointments: Do not miss any scheduled post-operative appointments, as these are crucial for your dentist to assess your healing.
References
[1] U.S. Department of Health and Human Services. (n.d.). The 2020 Surgeon General’s Report on Smoking and Health – Chapter 9: Oral Health. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK553942/
[2] American Academy of Implant Dentistry. (n.d.). What are dental implants?. Retrieved from https://www.aaid.com/dental_implants/what_are_dental_implants.html


Leave a Reply
Share your thoughts or ask a question about dental implants. Your email address will not be published.