Imagine investing in a solution that restores your smile and confidence, only to wonder years down the line: Can a dental implant get infected years after placement? It’s a valid and important question for anyone with or considering dental implants. While dental implants boast a remarkably high success rate, they are not entirely immune to complications, even long after their initial placement. The unfortunate truth is, yes, a dental implant can develop an infection, sometimes many years after it has been successfully integrated into your jawbone. This article will delve deep into the causes, symptoms, prevention, and treatment of late-stage dental implant infections, ensuring you have all the knowledge you need in 2026 to protect your investment and maintain optimal oral health.
Key Takeaways
- Late-stage infections are possible: Even years after successful integration, dental implants can become infected, a condition known as peri-implantitis.
- Poor oral hygiene is a primary culprit: Just like natural teeth, implants require diligent cleaning to prevent bacterial buildup.
- Recognize the signs: Swelling, pain, bleeding, and gum recession around the implant are critical warning signs.
- Prevention is paramount: Regular dental check-ups, excellent home care, and avoiding risk factors like smoking are essential.
- Early intervention is key: Prompt diagnosis and treatment significantly improve the prognosis for an infected implant.
Understanding Dental Implants and the Risk of Infection
Dental implants have revolutionized tooth replacement, offering a durable and aesthetically pleasing alternative to traditional bridges and dentures. They are surgically placed titanium posts that fuse with the jawbone (a process called osseointegration), acting as stable anchors for crowns, bridges, or full-arch prostheses. For many, they are a lifelong solution, restoring chewing function and appearance.
However, the oral cavity is a complex environment teeming with bacteria. While our bodies are generally good at keeping these bacteria in check, any foreign body, including a dental implant, can potentially become a site for bacterial colonization and subsequent infection. The period around the implant is particularly vulnerable.
What is Peri-Implantitis?
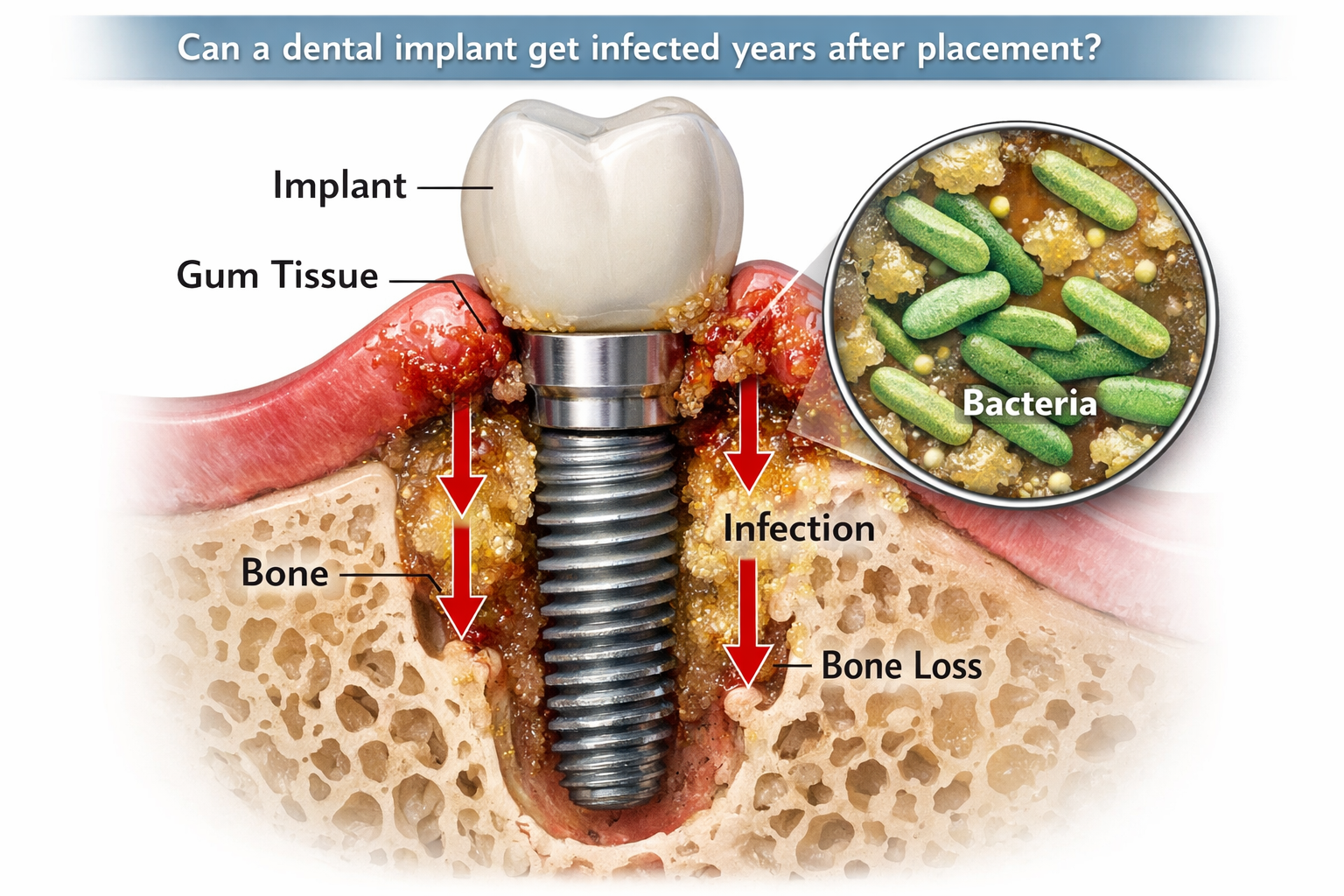
The most common form of late-stage dental implant infection is peri-implantitis. This condition is essentially the implant equivalent of periodontal disease (gum disease) that affects natural teeth. It’s an inflammatory condition that impacts the soft tissues (gums) and hard tissues (bone) surrounding an osseointegrated dental implant [1].
Initially, it might manifest as peri-implant mucositis, which is an inflammation of the soft tissues around the implant without bone loss. If left untreated, peri-implant mucositis can progress to peri-implantitis, characterized by inflammation accompanied by progressive loss of the supporting bone around the implant. This bone loss is particularly concerning because it can ultimately lead to implant mobility and failure.
“Peri-implantitis is a serious condition that can compromise the long-term success of dental implants, making early detection and intervention crucial for preserving both the implant and overall oral health.”
Why Can a Dental Implant Get Infected Years After Placement?
It might seem counterintuitive for an implant that has been stable for years to suddenly develop an issue. However, several factors can contribute to an infection developing long after the initial healing period. Think of it this way: even a healthy tree can get sick years into its life if its environment changes or it’s exposed to new threats.
The oral environment is dynamic, and various influences can lead to an infection around an implant over time. It’s not usually a sudden event but rather a gradual process that can escalate if unchecked.
Common Causes and Risk Factors for Late-Stage Implant Infections
Understanding the root causes and risk factors is the first step in prevention. Many of these factors are interconnected and can exacerbate each other.
1. Poor Oral Hygiene
This is perhaps the most significant and preventable cause. Just like natural teeth, dental implants require meticulous daily cleaning. Bacteria accumulate in plaque around the implant crown and along the gum line. If this plaque isn’t removed regularly, it can harden into tartar, irritate the gums, and lead to an inflammatory response. Over time, these bacteria can invade deeper tissues, causing peri-implantitis and bone loss.
- Plaque Buildup: The primary culprit.
- Lack of Regular Brushing and Flossing: Allows bacteria to thrive.
- Infrequent Professional Cleanings: Dental professionals can remove hardened plaque (calculus) that you can’t remove at home.
2. Smoking and Tobacco Use
Smoking is a well-established risk factor for both periodontal disease and peri-implantitis. Tobacco products restrict blood flow to the gums, impairing the body’s ability to heal and fight off infection. Smokers are significantly more likely to develop peri-implantitis and have a higher rate of implant failure [2]. The toxins in tobacco also promote bacterial growth and hinder immune responses.
3. Untreated Periodontal Disease
If you had gum disease before getting implants and it wasn’t adequately treated, or if new gum disease develops around your natural teeth, the bacteria responsible can migrate to your implant sites. This makes individuals with a history of periodontitis more susceptible to peri-implantitis [3]. It’s crucial that any existing gum disease is under control before implant placement and that it remains so afterward.
4. Systemic Health Conditions
Certain systemic diseases can compromise your immune system or affect bone health, making you more vulnerable to infections:
- Diabetes: Poorly controlled diabetes can impair healing and immune function, increasing the risk of infection.
- Osteoporosis: While not a direct cause of infection, conditions affecting bone density can indirectly impact the long-term stability of the implant and its susceptibility to issues.
- Immunocompromised States: Conditions or medications that suppress the immune system can make fighting off bacterial infections more challenging.
5. Excessive Biting Forces (Occlusal Overload)
While not a direct cause of infection, excessive force on an implant (e.g., from teeth grinding or clenching, known as bruxism, or from an improperly aligned bite) can put stress on the implant and the surrounding bone. This mechanical stress can potentially lead to microtrauma, which might make the area more susceptible to inflammation and bacterial invasion, especially if combined with other risk factors. Wearing a nightguard can often mitigate the effects of bruxism.
6. Poorly Designed or Fabricated Prosthesis
In some cases, the crown, bridge, or denture attached to the implant might not be perfectly designed. Overhangs or ill-fitting margins can create areas where plaque and bacteria can accumulate easily and are difficult to clean effectively. This can significantly increase the risk of peri-implantitis. Similarly, an abutment-supported porcelain ceramic crown that isn’t perfectly sealed can harbor bacteria.
7. Allergic Reactions or Material Intolerance (Rare)
While extremely rare, some individuals might develop a reaction to the titanium alloy used in implants. This is generally identified much earlier, but chronic inflammation could theoretically contribute to a compromised environment around the implant over many years.
8. Residual Cement
When attaching the crown to the implant abutment, dental cement is used. If excess cement is left behind under the gum line, it can act as a foreign body, irritating the tissues and providing a rough surface for bacteria to attach, leading to inflammation and potentially infection. This is a common, though often overlooked, cause of peri-implantitis.
9. Lack of Regular Dental Check-ups
Regular visits to your dentist and hygienist are crucial. They can identify early signs of peri-implant mucositis before it progresses to peri-implantitis. Professional cleanings are vital for removing plaque and tartar that you might miss. If you have full-arch implants like all-on-4 dental implants, specialized cleaning techniques are often required. Learn more about the importance of regular care for your implants at dentalimplantsdallastx.com.
Recognizing the Signs: How to Tell if a Dental Implant is Infected
Early detection is key to successful treatment. Be vigilant and pay attention to any changes around your implant. If you notice any of these symptoms, contact your dentist or oral surgeon immediately.
| Symptom | Description | Severity |
|---|---|---|
| Pain or Discomfort | Unlike natural teeth, healthy implants shouldn’t typically cause pain. Any persistent aching, throbbing, or sharp pain around the implant or when chewing is a red flag. | High |
| Swelling or Redness | The gums around the implant appear red, puffy, or swollen. Healthy gums should be pink and firm. | Moderate |
| Bleeding | Gums that bleed easily when brushing, flossing, or even spontaneously are a sign of inflammation. | Moderate |
| Pus Formation | A yellowish or whitish discharge (pus) coming from around the implant or when pressing on the gums is a clear sign of active infection. 🤢 | High |
| Bad Taste or Bad Breath | Persistent bad breath (halitosis) or a foul taste in your mouth that doesn’t go away with brushing can indicate bacterial activity. | Low |
| Gum Recession | The gum tissue around the implant crown starts to pull back, exposing more of the implant or abutment. This often indicates underlying bone loss. | High |
| Loose or Wobbly Implant | A healthy implant should feel absolutely solid. If it feels loose, even slightly, it is a serious sign of advanced bone loss and imminent failure. This requires immediate dental attention. | Critical |
| Difficulty Chewing | If you experience discomfort or reduced chewing efficiency on the side of the implant, it could be due to inflammation or instability. | Moderate |
| Changes in Bite | If the implant crown feels different when you bite down, or your bite feels “off,” it could be a sign of underlying issues affecting the implant’s stability. | Moderate |
“Any sign of inflammation or discomfort around your dental implant, especially if it appears years after placement, warrants immediate professional evaluation.”
Diagnosis of Peri-Implantitis
When you visit your dentist with concerns, they will typically perform a thorough examination, which may include:
- Visual Inspection: Checking for redness, swelling, pus, and gum recession.
- Probing: Gently measuring the depth of the gum pocket around the implant with a special probe. Increased probing depths often indicate inflammation and potential bone loss.
- Radiographs (X-rays): X-rays are crucial for assessing the bone level around the implant. They can show if there has been any bone loss compared to previous X-rays, indicating peri-implantitis.
- Mobility Test: Gently checking if the implant itself is loose.
- Review of Medical History: Discussing any systemic conditions, medications, or lifestyle habits that could be contributing factors.
Treatment Options for Infected Dental Implants

The treatment approach for an infected dental implant will depend on the severity of the infection, the amount of bone loss, and the overall health of the patient. The goal is to eliminate the infection, reduce inflammation, and, if possible, regenerate lost bone.
1. Non-Surgical Treatment
For early stages of peri-implant mucositis or mild peri-implantitis, non-surgical approaches are often attempted:
- Mechanical Debridement: This involves thoroughly cleaning the implant surface and surrounding tissues to remove plaque and calculus. This can be done using specialized plastic or titanium instruments, ultrasonic scalers, or air-abrasive devices.
- Antimicrobial Therapy: Your dentist may prescribe oral antibiotics or apply antiseptic rinses (like chlorhexidine) to help control bacterial growth. Localized delivery of antibiotics directly into the gum pocket can also be an option.
- Improved Oral Hygiene Instruction: Re-education on proper brushing, flossing, and potentially using specialized brushes or water flossers for implants is critical. Check out our guide on the best water flosser for dental implants for more information.
2. Surgical Treatment
If the infection has progressed and there is significant bone loss, surgical intervention may be necessary. These procedures aim to clean the infected area more thoroughly and, if possible, regenerate bone.
- Access Flap Surgery: The gum tissue is carefully lifted (a “flap” is created) to expose the implant surface and the bone defect. This allows for thorough cleaning and debridement of the infected implant surface.
- Surface Decontamination: Various methods are used to clean and disinfect the implant surface, including lasers, air-abrasive particles, and chemical agents. The goal is to remove bacteria and toxins without damaging the implant itself.
- Bone Grafting: After the infection is cleared, if there’s significant bone loss, bone grafting procedures may be performed to encourage the regeneration of bone around the implant. This often involves placing bone graft material and covering it with a protective membrane. This is similar to bone grafts for dental implants used during initial placement.
- Resective Surgery (Implantoplasty): In some cases, if the implant surface is rough and harbors bacteria, a procedure called implantoplasty may be performed to smooth the implant surface, making it easier to clean and less prone to bacterial adhesion.
- Implant Removal: In severe cases where the infection cannot be controlled, or if there is extensive, irreversible bone loss leading to implant mobility, the implant may need to be removed. This is often a last resort, but sometimes necessary to prevent further damage to the jawbone. After removal, a healing period is required, and future options for tooth replacement can be discussed.
Preventing Late-Stage Dental Implant Infections
Prevention is always better than cure, especially when it comes to the long-term success of your dental implants. Here are actionable steps you can take:
- Maintain Exemplary Oral Hygiene:
- Brush twice daily with a soft-bristled toothbrush and non-abrasive toothpaste.
- Floss daily, using dental floss specifically designed for implants or an interdental brush.
- Consider a water flosser to clean around the implant and under the gum line.
- If you have All-on-4 dental implants, specialized cleaning tools and techniques are essential.
- Regular Dental Check-ups and Professional Cleanings:
- Visit your dentist at least twice a year for check-ups and professional cleanings. These appointments are crucial for monitoring implant health, identifying early signs of trouble, and removing hardened plaque.
- For those with a history of gum disease or other risk factors, more frequent visits might be recommended.
- Quit Smoking: If you smoke, quitting is one of the most impactful steps you can take to protect your oral health and the longevity of your implants.
- Manage Systemic Diseases: If you have diabetes or other systemic health conditions, work closely with your physician to keep them well-controlled.
- Address Bruxism (Teeth Grinding): If you grind or clench your teeth, discuss this with your dentist. A nightguard can protect your implants from excessive forces.
- Choose Experienced Professionals: Ensure your dental implants are placed and restored by experienced and qualified dental professionals. Proper placement and a well-designed prosthesis are fundamental to long-term success. For comprehensive dental implant services, consider consulting experts like those at Dental Implants Dallas TX.
- Follow Post-Operative Instructions: Adhering to all post-operative care instructions immediately after implant surgery, including dietary restrictions (like 50 soft foods after dental implant) and avoiding certain activities, sets a strong foundation for healing.
My Experience and Advice
As a dental professional, I’ve seen firsthand how diligent home care can make a monumental difference. Patients who commit to regular brushing, flossing, and keeping their dental appointments rarely encounter late-stage infections. It’s an ongoing partnership between you and your dental team. Don’t be afraid to ask questions about the best cleaning tools or techniques for your specific implant setup. Your oral health is a journey, not a destination.
The Prognosis for Infected Implants in 2026
The prognosis for an infected dental implant largely depends on how early the peri-implantitis is diagnosed and treated.
- Early Intervention: If caught in the early stages (peri-implant mucositis or mild peri-implantitis), treatment is often successful, and the implant can be preserved with proper care and follow-up.
- Advanced Stages: For more advanced cases with significant bone loss, treatment becomes more complex, and the success rate of saving the implant decreases. While surgical interventions and bone grafting can be effective, there’s a higher risk of recurrence or eventual implant failure.
- Complete Failure: In cases of irreversible bone loss and mobility, the implant may need to be removed. Even then, after the site heals, it may be possible to place a new implant, provided there’s sufficient healthy bone.
It’s important to remember that dental technology and techniques are continually advancing. In 2026, we have access to more sophisticated diagnostic tools and a wider array of treatment options for peri-implantitis than ever before. However, the fundamental principles of prevention and early detection remain the most powerful tools in our arsenal.
Conclusion
The question, “Can a dental implant get infected years after placement?” regrettably has a “yes” answer. While dental implants are incredibly successful and durable, they are not immune to infection, even long after they have integrated into your jawbone. Peri-implantitis, the primary culprit, is an inflammatory condition that can lead to bone loss around the implant and, if left untreated, implant failure.
The good news is that with diligence and proactive care, the risk of such infections can be significantly minimized. Maintaining impeccable oral hygiene, attending regular dental check-ups, avoiding risk factors like smoking, and promptly addressing any unusual symptoms are your best lines of defense.
If you suspect your dental implant might be infected, do not delay. Contact your dentist immediately. Early diagnosis and intervention are critical to preserving your implant, protecting your oral health, and ensuring the longevity of your investment. Your dental team is your partner in maintaining a healthy, radiant smile for years to come. For more information about maintaining your oral health and exploring various dental solutions, visit our About Us page or explore our comprehensive blog.
References
[1] Renvert, S., Persson, G. R., & Pirih, F. Q. (2018). Peri-implantitis: a narrative review and proposed classification scheme. Journal of Oral & Maxillofacial Research, 9(3), e4.
[2] Strietzel, F. P., Reichard, S., & Wegner, P. K. (2017). Smoking and dental implants: A systematic review and meta-analysis. Journal of Oral & Maxillofacial Surgery, 75(5), 986-997.
[3] Koldsland, O. P., Scheie, A. A., & Aass, A. M. (2010). Prevalence of peri-implantitis related to severity of periodontal disease. Journal of Clinical Periodontology, 37(11), 1016-1023.
Dental Implant Infection Risk Evaluator (2026)
Assess your potential risk for developing peri-implantitis years after placement. This is for informational purposes only; consult a dental professional for personalized advice.

Leave a Reply
Share your thoughts or ask a question about dental implants. Your email address will not be published.